Recent Updates on Tinnitus Management
Article information
Abstract
In this comprehensive review, we discuss recent updates on tinnitus evaluation and treatment. Tinnitus evaluation commences with comprehensive medical history taking and audiological evaluation, which can provide valuable insight into the nature and extent of auditory disturbances. Additionally, tinnitus evaluation includes investigation of psychosomatic comorbidities to determine the intricate interplay between psychological factors and tinnitus perception. Various therapeutic approaches are available to minimize the burden of tinnitus. Cognitive behavioral therapy reshapes negative thought patterns and behaviors that are closely associated with tinnitus-induced distress. Acceptance and commitment therapy fosters mindfulness and value-aligned actions to address emotional effects. Tinnitus retraining therapy combines counseling and sound therapy for habituation. Tailor-made notched music therapy offers customized auditory experiences for symptom relief. Hearing aids and cochlear implants compensate for hearing loss and associated stress. Both neuromodulation and neurofeedback may be potentially useful. The role of pharmacotherapy and dietary supplements remains uncertain. Physiotherapy and head-neck manipulation relieve tinnitus associated with orofacial factors. Virtual reality, smartphone applications, and photobiomodulation may serve as novel therapeutic avenues. Although promising interventions are available, further research is warranted to confirm their effectiveness and long-term effects.
Introduction
Tinnitus is not an uncommon symptom; instead, it is a prevalent condition that does not vary significantly based on gender but tends to increase with age. The annual incidence of tinnitus is approximately 1%. About 14% of adults experience some form of tinnitus, while 2% experience a more severe manifestation [1].
Tinnitus is the conscious perception of a tonal or composite noise without any identifiable external acoustic source. More recently, a novel concept known as tinnitus disorder has emerged [2]. Tinnitus disorder can be defined when tinnitusassociated emotional and/or cognitive dysfunctions, along with autonomic arousal leading to behavioral changes and functional disability, are observed.
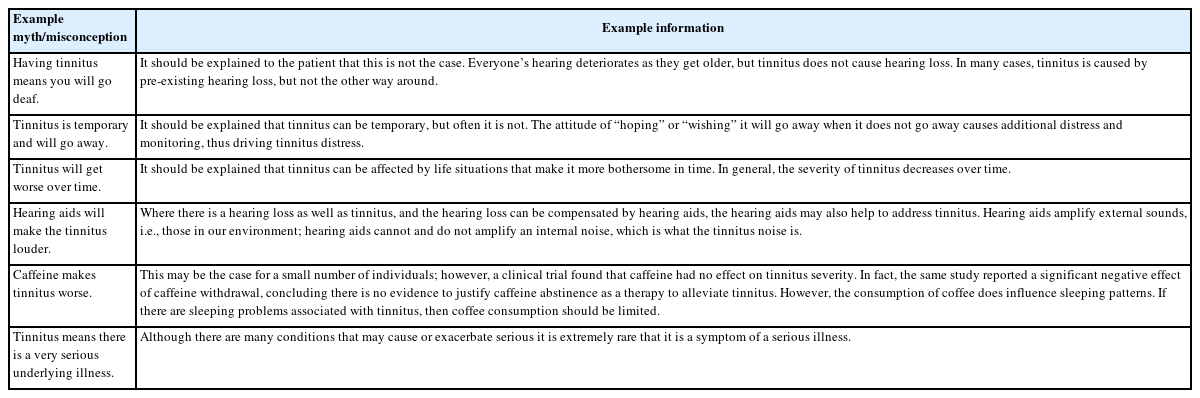
In 2014, a clinical practice guideline for tinnitus was published, serving as a fundamental resource for diagnosing and treating this condition [3]. Additionally, chronic tinnitus guidelines were released in Japan and Europe in 2019, England in 2020, and Germany in 2022 [4-7]. Table 1 summarizes these guidelines, which can significantly aid in the more effective management of tinnitus patients. The main focus of this article is to concisely present the updated information, primarily centered around these guidelines, along with recently published randomized controlled trials, meta-analyses, systematic reviews, and significant observational studies related to tinnitus management.
Basic Assessment for Tinnitus
A thorough medical history assessment is crucial. Following that, the German guideline outlines essential steps for a com-prehensive tinnitus evaluation, including ear endoscopy, puretone audiometry, speech audiometry, tympanometry, auditory brainstem response, and otoacoustic emissions (Fig. 1). Additionally, tests for spontaneous nystagmus and provocative nystagmus should be performed, along with a crucial manual examination of the masticatory apparatus and the cervical spine [4]. In Japan, the pitch match test and loudness balance test are also recommended [5]. In addition, various additional hearing tests can be considered to diagnose decreased sound intolerance, extended-high frequency hearing loss, endolymphatic hydrops, auditory neuropathy, hidden hearing loss, and so forth [8]. In other words, a comprehensive diagnostic workup involving audiological assessment and identification of hearing loss should be carried out as the initial step.
Additionally, concurrent psychosomatic comorbidities such as anxiety, depression, and severe stress should be assessed [8-10]. It is worth noting that the Tinnitus Handicap Inventory (THI) is recommended for diagnosing tinnitus in the Japanese guideline [5]. The guideline also suggests utilizing questionnaires such as the Tinnitus Questionnaire, THI, Tinnitus Reaction Questionnaire, and 36-Item Short Form Survey (SF-36) for quality of life. THI, in particular, has demonstrated a strong correlation with psychological assessment surveys [9].
For imaging studies, imaging can be obtained if tinnitus localizes to one ear, pulsatile tinnitus, focal neurological abnormalities, or asymmetric hearing loss [3,5].
Overview of Current Tinnitus Treatments
This review explores a wide spectrum of tinnitus treatments, encompassing psychotherapies such as cognitive behavioral therapy, acceptance and commitment therapy, and tinnitus retraining therapy, sound-based therapies, hearing devices including hearing aids (HA) and cochlear implants (CI) for profound hearing loss, neurofeedback and neuromodulation techniques, the current status of pharmacotherapy, and emerging digital solutions.
Cognitive behavioral therapy for tinnitus
All of the recent guidelines strongly endorse cognitive behavioral therapy (CBT) [3-5]. CBT aims to identify and modify negative thought patterns and behaviors by recognizing the interconnectedness of thoughts, emotions, and actions. It challenges distorted beliefs and substitutes them with more balanced ones, employing methods such as cognitive restructuring, behavior activation, exposure therapy, and problemsolving (Table 2). CBT encompasses cognitive restructuring, behavior activation, exposure therapy, and problem-solving techniques.
Recent studies even challenge the notion that CBT only reduces annoyance and distress, showing it can also lower tinnitus loudness [11]. A Cochrane review notes CBT’s potential to alleviate tinnitus’s impact on quality of life, though longterm effects remain uncertain [12]. While CBT might alleviate depression symptoms, its effects on anxiety, health-related quality of life, and changing negative tinnitus interpretations need more investigation [12]. Internet-based CBT is promising for addressing tinnitus distress [9]. As CBT’s potential unfolds, including group sessions and internet-based approaches, tinnitus management holds promise [13,14].
Acceptance and commitment therapy and mindfulness
Acceptance and commitment therapy (ACT) can indeed be considered a second-generation form of CBT. ACT encourages individuals to accept their thoughts and emotions without judgment (Fig. 2). Instead of battling unwanted feelings of tinnitus, ACT guides individuals toward values-driven actions that enhance overall well-being. By cultivating mindfulness, individuals can increase awareness of their thoughts, emotions, and bodily sensations, fostering a non-reactive stance to these experiences [15]. Some studies reported that ACT was superior to tinnitus retraining therapy (TRT) or internet-based CBT [16,17]. However, a recent meta-analysis showed that there is currently insufficient evidence to recommend the use of ACT or mindfulness for improving hearing-related distress or psychological well-being in people with audiological problems because these effects are limited to short-term [18].
Tinnitus retraining therapy
TRT is an approach aimed at habituating to tinnitus by reducing its auditory, emotional, and autonomic impact. This technique incorporates both counseling and sound therapy utilizing broadband noise [4]. TRT can be employed as a longterm intervention [4]. For TRT, the use of a sound generator is not deemed essential, as it does not offer any additional benefits [4].
A meta-analysis involving 1,345 patients revealed that combining TRT with drugs led to higher response rates and reductions in THI scores compared to treatments involving drugs alone [19]. However, it is worth noting that the quality of evidence could have been more robust due to the limited number of studies and the potential for bias [19]. In a comparative study with TRT, counseling alone was mentioned as “partial” TRT, standard of care; results indicated no significant differences between TRT or partial TRT compared to standard of care across various tinnitus-related quality of life measures [20]. Similarly, a study divided patients into three groups: counseling only, counseling and total masking, and counseling and partial masking. The extent of improvement varied among groups, but no significant differences were observed, and individual differences were likely influenced by expectations [21].
Tailor-made notched music therapy & music therapy
Tailor-made notched music therapy (TMNMT) uses tinnitus-frequency removed music, and the mechanism of action is associated with the enhancement of lateral inhibition. It may be helpful, especially for individuals who prefer music-based interventions. However, the German guideline recommends that TMNMT should not be used in chronic tinnitus because it is no more effective than music and there is also potential harm [4]. In most recent studies, TMNMT did not differ in efficacy from other interventions, including conventional music or randomly removed frequency, counseling, and TRT [22-25].
In a double-blinded randomized controlled trial, 104 patients with chronic subjective tinnitus examined the effectiveness of TMNMT compared to ordinary music therapy until 6 months [22]. Divided into treatment and control groups, participants were assessed at 1, 3, and 6 months. However, THI and visual analog scale (VAS) were similar. Similarly, in a comparison between TMNMT and TRT, both TMNMT and TRT significantly reduced THI scores over a 3-month treatment period [23]. A study comparing TMNMT, conventional music therapy, and counseling revealed that all three interventions contributed to decreased THI scores over time, but there were no significant differences [14].
Hearing aids
All of the guidelines recommend HA for individuals with hearing loss and tinnitus [3-5]. HA compensates for auditory deprivation, reduces attentional focus on tinnitus by amplifying the ambient environmental sounds, and reverses central changes related to tinnitus in the auditory brain. It also alleviates tension associated with straining to hear, reducing stress. However, research has shown a significant amount of disagreement regarding the effectiveness of amplification methods, the inclusion of notched filter, frequency lowering techniques, and the use of combined sound generators in treating tinnitus.
For patients with mild-to-moderate hearing loss and tinnitus, no significant difference was observed in the comparison between amplification with conventional HA and the use of a notched filter to exclude the tinnitus frequency band, enhancing lateral inhibition [26]. When comparing wide dynamic range compression (WDRC) with frequency compression, most patients reported greater satisfaction with the sound quality of WDRC, leading to the suggestion that traditional amplification methods are more effective in patients with hearing loss accompanied by tinnitus [27]. In contrast, over 3 months of HA use, no differences in THI were observed among WDRC, linear frequency transposition, and frequency translation, all of which showed significant reductions in the THI, and the tinnitus suppression effect of the HA was maintained even after discontinuation [28]. Comparisons between combined HA with sound generators with conventional HA did not show significant differences in their effects in most studies until now [29,30].
Cochlear implant
According to the guidelines, if HA is insufficient to address hearing loss, CI should be considered, even in cases of unilateral hearing loss [4,5]. CI has shown promising results in improving tinnitus-related distress and quality of life. A systematic review analyzing 1,285 patients demonstrated significant enhancements in tinnitus-related measures such as THI, VAS, and Tinnitus Questionnaire scores [31]. Recent studies reported the advantages of CI for single-sided deafness, underscoring its positive impact on speech perception, tinnitus control, sound localization, and overall quality of life [32]. Another avenue of exploration is CI programming for tinnitus suppression, which indicated potential benefits in reducing tinnitus severity. Research suggests that various parameters, including electrode numbers and stimulation levels, could contribute to effective tinnitus management [33]. Moreover, using smartphone apps, such as ReSound Tinnitus Relief, in CI users exhibited a mixed but encouraging outcome, with some users experiencing relief from tinnitus [34,35]. However, further validation and optimization are needed to harness the full potential of these interventions for tinnitus management.
Neuromodulation
The guidelines advise against neuromodulation due to a lack of placebo-controlled studies or proven efficacy [3-5]. Transcranial direct current stimulation (tDCS) and repetitive transcranial magnetic stimulation (rTMS) are representative neuromodulation techniques, often targeting the left auditory and prefrontal cortex. Studies consistently show positive tinnitus suppression outcomes when targeting the temporoparietal junction midway between T3 and P3 or between T4 and P4 [36]. Anodal and cathodal stimulation types are used in tDCS to modulate excitability, with potential side effects including fatigue, tingling, skin burns, headaches, itching, and insomnia. Notably, six sessions of tDCS (F4: anode, F3: cathode, intensity: 1.5 mA) were found most effective for tinnitus [37]. However, high-definition-tDCS (HD-tDCS), delivering more intense stimulation through smaller electrodes, has not yielded the expected results [38]. A recent dual-site tDCS study showed no difference in TFI between active and sham groups, suggesting a placebo effect [39]. Transauricular vagus nerve stimulation (tVNS) is promising for tinnitus relief, yet methodological limitations necessitate robust trials for conclusive evidence [40,41].
The emerging trend of bimodal stimulation has gained attention in tinnitus management, encompassing multisensory approaches that include visual, auditory, and tactile elements. One of the simplest methods for achieving bimodal stimulation involves combining neuromodulation with sound therapy. Furthermore, the combination of different stimulation modes has demonstrated promise in reducing tinnitus severity, as demonstrated by the Leniere device, which integrates sound and tongue electrical stimulation. This approach resulted in a notable 14.6-point reduction in the THI scores after 12 weeks of use. Notably, patient satisfaction with bimodal neuromodulation settings has been consistently high, ranging between 70% and 80% [42-44].
Neurofeedback
Neurofeedback holds promise in alleviating tinnitus distress and its associated effects, supported by studies demonstrating favorable results by manipulating alpha and delta wave patterns. Nonetheless, the certainty of these findings is constrained by the need for more extensive research in this domain [45]. Recent systematic reviews and randomized trials have highlighted notable reductions in tinnitus intensity and distress following repeated neurofeedback sessions focusing on alpha/delta and beta/theta ratios. While the efficacy of alpha/delta neurofeedback is evident, additional investigations are necessary to establish its distinct role as a viable tinnitus treatment [45,46].
Pharmacotherapy
In guidelines, insufficient data supports the effectiveness of drug treatments for tinnitus [3-5]. Some drugs such as betahistine, Ginkgo biloba extract, the combination of G. biloba extract plus St. John’s wort, antidepressants, benzodiazepines, zinc, melatonin, cannabis, oxytocin, steroids, and gabapentin have been found ineffective for chronic tinnitus, and these drugs should not be recommended [4,47]. Regarding G. biloba extract, the combination of G. biloba extract and HA led to significant improvements in tinnitus severity [48].
In addition to the mentioned drugs, a randomized-controlled trial evaluated acamprosate, an antagonist of glutaminergic activity, and a gamma-aminobutyric acid (GABA) agonist used for alcoholism treatment for tinnitus. The study found that participants receiving acamprosate experienced significant reductions in tinnitus-related scores and positive electrophysiological changes in cochlear and auditory nerve function [49]. As for methylenedioxymethamphetamine (MDMA), a study exploring its effects on tinnitus perception indicated that MDMA had similar effects to placebo in terms of tinnitus perception. However, after a higher dose, it showed reduced annoyance and altered brain connectivity. Further research is warranted to explore the potential of MDMA as a tinnitus treatment [50].
A network meta-analysis for pharmacotherapy for primary tinnitus showed that medications with brain-acting effects (e.g., amitriptyline, acamprosate, gabapentin) and those with anti-inflammation/antioxidant effects (e.g., intra-tympanic dexamethasone plus oral melatonin) were associated with better improvement in tinnitus severity and response rates compared to placebo. Additionally, amitriptyline demonstrated the highest improvement in severity [51].
Overall, the efficacy of pharmacotherapy for tinnitus remains uncertain. The field is characterized by positive and inconclusive findings, necessitating more rigorous research to better understand the potential benefits and risks of these interventions. However, as described in the guideline, it is essential not to overlook the fact that drugs can still be used to treat conditions related to tinnitus, such as anxiety and depression, following established guidelines (Table 3).
Dietary supplements
Recent German guideline advises against using dietary supplements like vitamins, traditional herbal medicine, minerals, homeopathy, and lipoflavonoids for tinnitus treatment due to insufficient evidence of effectiveness [4]. Similarly, an online survey-based study revealed that while caffeine, alcohol, and salt could slightly impact tinnitus severity for some participants, the effects were generally mild. The researchers emphasized that dietary changes are not a primary treatment for chronic tinnitus in the general population, although some individuals might see meaningful effects [52].
The author concurs with these perspectives. While dietary supplements are essential for maintaining health, tinnitus is influenced by factors beyond nutrition. Most supplement research relies on large-scale studies such as the National Health and Nutrition Examination Survey. A recent US study linked low blood manganese to tinnitus frequency and impact, while serum zinc and vitamin B12 had no significant links to tinnitus [53]. This underscores the need for more research into manganese supplementation for tinnitus patients.
Similarly, a Korean study using the Korea National Health and Nutrition Examination Survey (KNHANES) found no connection between hypozincemia and tinnitus [54]. Additionally, middle-aged individuals (ages 51–60 years) with tinnitus showed lower vitamin B2 intake—and reduced water, protein, and vitamin B3 intake related to tinnitus-related annoyance. The study underscores proper nutrition’s importance in managing tinnitus and highlights the necessity for further research [55].
Other surgeries
Apart from CI, one of the most commonly performed surgeries for tinnitus is sigmoid sinus resurfacing surgery. Patients with venous pulsatile tinnitus experience tinnitus synchronized with their heartbeat, and ipsilateral neck compression directly alleviates tinnitus and improves low-frequency hearing loss. The elimination of pulsatile tinnitus after compression has been reported as an excellent prognostic factor following repair of the sigmoid sinus [56]. The results of the water occlusion test may also predict the surgical outcome after resurfacing surgery [57].
Additionally, middle ear myoclonus (MEM) is another condition that can be surgically treated to ameliorate tinnitus. A simple transcanal endoscopic resection of the stapedial tendon and/or tensor tympani tendon is necessary for this procedure [58]. On the other hand, intratympanic Botox injection has been introduced and is under study. It could be applied to patients with MEM if positive results are revealed [59].
Physiotherapy and head and neck manipulation
Tinnitus, often influenced by orofacial factors like temporomandibular disorders (TMD) or neck pain, can benefit from physiotherapy and head and neck manipulation [60]. TMD pain reduction mediates the improvement of somatic tinnitus after orofacial treatment, emphasizing the link between these factors [60]. Orofacial treatment or combining cervico-mandibular manual therapies with exercise and education yields better outcomes for TMD-associated tinnitus [61,62]. Baseline tinnitus severity, tinnitus-related handicap, and pressure pain thresholds over the temporalis muscle significantly predict treatment effectiveness in TMD-related tinnitus [63]. A pilot study explored the effectiveness of EMS (exercise to improve muscle strength, motion of joints, and stretch training) as a somatosensory stimulation therapy for somatosensory tinnitus symptoms [64]. The study findings suggest that EMS therapy is effective and safe for improving somatosensory tinnitus symptoms, with sustained therapeutic effects over weeks. Together, physiotherapy and head and neck manipulation have shown promising results in ameliorating tinnitus severity in patients with TMD, somatic tinnitus, and related conditions.
Others
In the rapidly expanding digital hearing healthcare market, combining virtual reality and sound therapy and treatments through smartphone applications like sound therapy and CBT is proving promising [65,66]. Furthermore, new treatment approaches are being introduced, including methods like photobiomodulation [67]. Although current meta-analyses do not indicate significant therapeutic effects in acupuncture, there remains a potential for notable individual differences and placebo effects [68,69].
Conclusion
When treating patients with tinnitus, the initial steps involve conducting a detailed medical history assessment, checking for abnormalities in the auditory system, identifying any accompanying psychological issues, and evaluating the severity of tinnitus discomfort through auditory tests and questionnaires.
Table 4 provides a concise overview of current tinnitus treatments, distinguishing between established recommendations and areas warranting additional research. Among the currently utilized treatments, those incorporating counseling, such as CBT, ACT, mindfulness, or TRT, have proven to be the most effective and should be prioritized. Other methods like TMNMT or music therapy have limited efficacy. Recommending HA or CI is beneficial for patients with tinnitus accompanied by hearing loss.

Summary of non-pulsatile tinnitus treatments: current recommendations and areas requiring further research
Certain medications, such as amitriptyline, acamprosate, gabapentin, intratympanic dexamethasone, and melatonin, have been reported to show some effects potentially. However, as there is no definitive medication to treat tinnitus, routine use of these drugs should be avoided. Nevertheless, in cases where tinnitus is accompanied by insomnia, depression, anxiety, or other conditions, referring to relevant guidelines can lead to appropriate medication usage.
While no specific nutritional supplements are recognized exclusively for tinnitus treatment, deficiencies in specific nutrients vary depending on the presence of tinnitus. Neuromodulation techniques like rTMS, tDCS, and tVNS should not be routinely applied to all patients, but they do show efficacy in some instances. Therefore, their application should be tailored to individual patients, and discussions about more suitable stimulation methods and targeted areas are necessary. Neurofeedback has shown positive treatment results recently, suggesting a promising outlook. In cases where tinnitus is accompanied by temporomandibular joint or neck problems, physiotherapy or manual medicine appears helpful.
Acknowledgements
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI21C1574040021).
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Ho Yun Lee. Data curation: Ho Yun Lee, Da Jung Jung. Formal analysis: Ho Yun Lee. Funding acquisition: Ho Yun Lee. Methodology: Ho Yun Lee, Da Jung Jung. Supervision: Ho Yun Lee. Validation: Ho Yun Lee, Da Jung Jung. Visualization: Ho Yun Lee. Writing—original draft: Ho Yun Lee. Writing—review & editing: Ho Yun Lee. Approval of final manuscript: Ho Yun Lee, Da Jung Jung.