Introduction
Acute coalescent mastoiditis is known as a complication of acute otitis media. Development of antibiotics led to rapid decrement of acute mastoiditis, reporting its incidence as low as 0.004% in the 1980s.1) However, acute otitis media associated with suppurative complications such as subperiosteal abscess, facial palsy, and intracranial complication are yet on a constant rise due to recent increase of antibiotic-resistant bacteria.2-6) Several studies have reported satisfying treatment outcomes of acute coalescent mastoiditis with proper drainage, ventilation and intravenous antibiotics although other authors have questioned the necessity of mastoidectomy.
Here, we report our experience in treatment of acute otitis media-induced acute mastoiditis associated with subperiosteal abscess in child and adult, discuss proper management of the disease, and review its literature.
Case Report
Case 1 (Child)
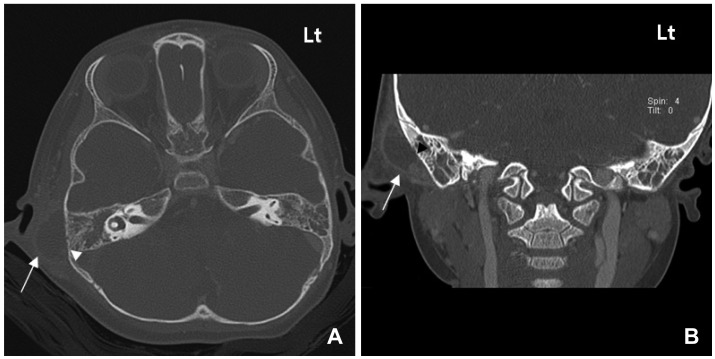
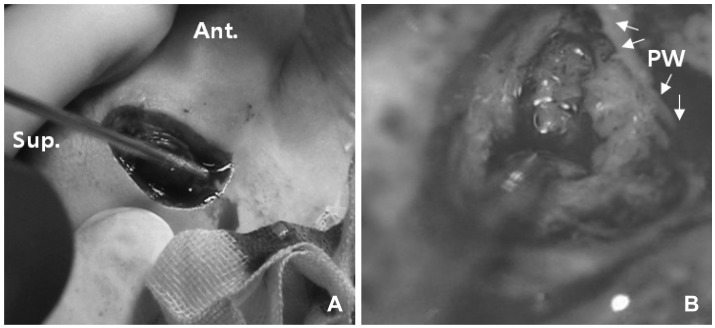
A 2 year old female admitted to the emergency department due to 2 days of right postauricular area swelling. The patient was previously treated with antibiotics for a week at a local clinic for acute otitis media. Despite antibiotic treatment, the patient suffered from right otalgia and fever upon admission. Through physical examination, bulging of the tympanic membrane and erythematous change and swelling of the right postauricular area with tenderness were noticed. Further evaluation by temporal bone CT revealed soft tissue density filling the right middle ear and mastoid cavity with erosion of the cortical bone along with formation of subperiosteal abscess (Fig. 1). Under the impression of acute mastoiditis with subperiosteal abscess, percutaneous aspiration was performed on the postauricular area resulting in 3 cc of purulent fluid. The procedure was followed by incision and drainage (I & D) and oral antibiotics were prescribed to the patient. On third day after I & D, the patient showed persistent redness, tenderness, and swelling of the postauricular area (Fig. 2) and injected bulging tympanic membrane, regardless of the treatment. Therefore, it was postulated that I & D and oral antibiotics were inadequate and the patient was admitted to our department for intravenous antibiotics therapy.
On the second day of hospitalization, the patient underwent surgical treatment of right simple mastoidectomy and ventilation tube insertion because of consistent symptoms and physical findings in spite of 2 days of intravenous antibiotic treatment. Intraoperative finding showed massive granuloma beneath the postauricular area and in the mastoid cavity (Fig. 3). Erosion of cortical bone was also noticed after Palva flap elevation. Intraoperative culture study resulted in Streptococcus pneumoniae which was only susceptible to vancomycin. Intravenous antibiotic treatment with vancomycin was immediately initiated and the child was discharged after 13 days of surgery without any postoperative complications. During the 5 month follow up, the patient showed no signs or symptoms of recurrence.
Case 2 (Adult)
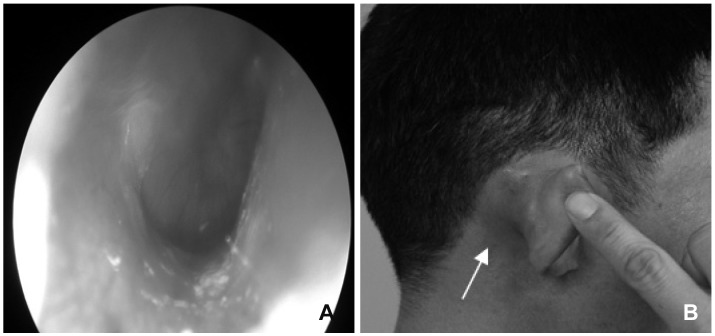
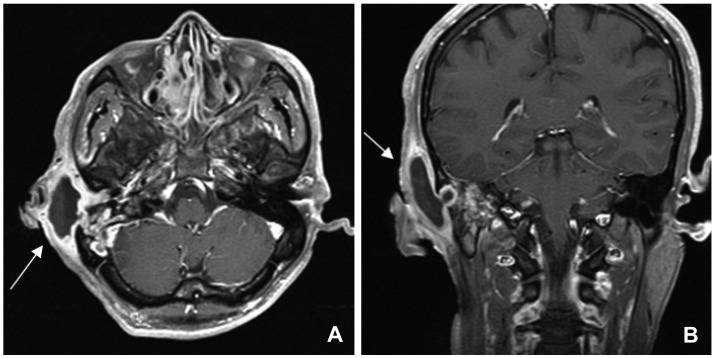
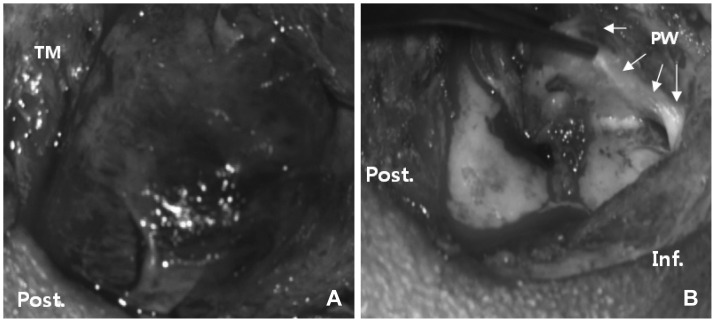
A 41 year old male visited the emergency department suffering from right otalgia for 1 month. The patient had no known medical history and complained of hearing impairment and otalgia on the right side. Physical examination showed injected bulging tympanic membrane associated with right postauricular swelling, redness and tenderness (Fig. 4). Further evaluation through pure tone audiometry revealed a mixed hearing loss on the right side with 60 dB air conduction level and 30 dB air-bone gap. Radiologic examinations of temporal bone CT and MRI showed soft tissue density filling the right middle ear and mastoid cavity with cortical bone erosion. Subperiosteal abscess was also detected over the cortical bone (Fig. 5). The patient was admitted and treated with I & D and antibiotics. Culture study that was processed during I & D revealed penicillin-sensitive Streptococcus pneumoniae. Even after 7 days of hospitalization, there were no signs of improvement. Thus, on the 8th day of hospitalization, right canal wall up mastoidectomy and tympanoplasty were performed. During the operation, granulation tissue in the mastoid cavity and middle ear cavity was detected and removed completely (Fig. 6). The patient was discharged after a week of surgery with significant improvement of previous symptoms and physical findings. No suspicious signs of recurrence were encountered during the 1 year follow up.
Discussion
Acute mastoiditis with subperiosteal abscess frequently occurs as a complication of acute otitis media and the incidence rate had decreased in accordance with the development of antibiotics. However, in the past 20 years it is on the rise again probably due to the growth of antibiotics-resistant bacteria.2-6)
Generally, subperiosteal abscess occurs in children who had been diagnosed with acute otitis media. The disease may be suspected through its characteristic features of injected bulging tympanic membrane, persistent otalgia and fever despite oral antibiotics eventually advancing to postauricular swelling, erythematous change, and tenderness. Temporal bone CT uniquely features soft tissue density in the middle ear and mastoid cavity, erosion or defect of cortical bone of the mastoid cavity, and contrast-enhanced subperiosteal shadows. In some cases, MRI may be necessary to determine intracranial complications.5) Similarly, in the second case, MRI was performed to detect possible intracranial involvement and differentiate other diagnosis since the occurrence rate of acute otitis media associated with complications is relatively low in adults.
Before the development of antibiotics, surgery was the treatment of choice for acute mastoiditis. Early surgical management and the use of proper antibiotics confirmed by culture study had been advocated to reduce morbidity and mortality especially in cases of acute mastoiditis associated with complications.
Recently, many studies have proved that proper I & D, ventilation, and intravenous antibiotic are sufficient treatment methods for acute mastoiditis. Favorable outcomes have been reported after treatment of patients under 2 years of age through ventilation tube insertion, I & D, and aspiration combined with intravenous antibiotics.7-10) These less invasive treatment modalities should be considered before mastoidectomy to reduce anesthetic risks and due to concerns of possible adverse effects of the ventilation system in the temporal bone by early mastoidectomy. However, the surgical treatment should be considered in cases of disappointing treatment outcomes with intravenous antibiotics, I & D, myringotomy or ventilation tube insertion. Mostly, studies have reported to proceed operation after 48 to 72 hours of conservative treatment.6-10) The most common causative organism of acute mastoiditis is Streptococcus pneumoniae2,4,9) which is often reported to be resistant to certain antibiotics. Therefore, proper antibiotic selection is also of great importance. In the first case, simple mastoidectomy was performed after 3 days from the patient's emergency room visit due to her exacerbating condition even after I & D and oral antibiotics. As in this case, surgical intervention might be considered when there is no clinical improvement within 2-3 days after I & D and antibiotic treatment. Other indications for simple mastoidectomy and ventilation tube insertion suggested in several studies11) are 1) patient over 30 months old and 15 kg, present with protruded mastoid abscess 2) associated with intracranial co-morbidities 3) diagnosed with cholesteatoma, and 4) failure of 2 week antibiotic treatment in patients with granuloma and suppurative otorrhea.
In the second case, the adult patient also underwent mastoidectomy because the patient's condition did not adequately respond to I & D and intravenous antibiotics. Acute coalescent mastoiditis in adults is often associated with chronic otitis media or cholesteatoma12) that mastoidectomy is also known to be performed to determine other possible causes of acute mastoiditis.
In conclusion, the clinician should always be aware that patients diagnosed with acute otitis media may be accompanied by suppurative complication regardless of age. In addition, early diagnosis and treatment should be carried out with assistance of its characteristic clinical manifestations and unique image findings. Treatment modalities include administration of intravenous antibiotics, pain control, and early consideration of myringotomy, ventilation tube insertion, or I & D. If the treatment effect is in question, mastoidecomy should be performed to prevent possible progression and avoid additional complications.