 |
 |
- Search
| J Audiol Otol > Volume 21(1); 2017 > Article |
|
Abstract
Background and Objectives
Viral and vascular disorders are considered to be a major cause of idiopathic sudden sensorineural hearing loss (ISSNHL). Lipoprostaglandin E1 (lipo-PGE1) has vasodilating activity and has been used to treat ISSNHL. The purpose of this study was to determine the specific therapeutic effects of lipo-PGE1 and compare them to other treatment modalities for ISSNHL.
Subjects and Methods
The study group had 1,052 patients diagnosed with ISSNHL. All were treated with steroid, carbogen inhalation, stellate ganglion block (SGB), or PGE1. The CP group (steroid, carbogen inhalation, and PGE1 injection; 288 patients) was treated with lipo-PGE1 and carbogen inhalation, the CS group (steroid, carbogen inhalation, and stellate ganglion block; 232 patients) with steroid, carbogen inhalation, and SGB, the C group (steroid and carbogen inhalation; 284 patients) with steroid and carbogen, and the control group (steroid only; 248 patients) with steroid only. Patients in the groups receiving lipo-PGE1 received a continuous infusion of 10 ┬ĄL lipo-PGE1.
Results
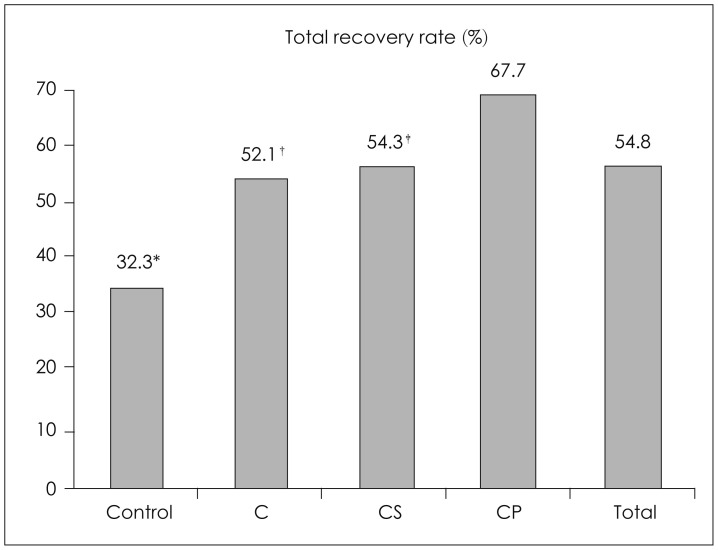
The overall recovery rate after treatment was 52.2%, and recovery rates by group were 67.7% in the CP group, 54.3% in the CS group, 52.1% in the C group, and 32.2% in the control group. Therefore, the therapeutic results in groups treated with lipo-PGE1 were better than results in other groups. The difference was statistically significant.
Idiopathic sudden sensorineural hearing loss (ISSNHL) is a sudden, rapid, progressive, partial or complete, unilateral sensorineural hearing impairment with occasional tinnitus or vertigo and unknown etiologic factors. The first description of ISSNHL as a clinical disease entity was in 1944 [1]. ISSNHL often leads to otologic emergencies requiring immediate and careful treatment and its incidence is approximately 5 to 20 per 100,000 people [2].
Vascular and viral mechanisms have been considered as major causes and pathophysiologies of ISSNHL and various vasodilators and antiviral agents are used as treatments. Many treatment methods have been proposed and used but no single successful method exists. Recently, carbogen inhalation, stellate ganglion block (SGB), and prostaglandin E1 (PGE1) have been used to treat ISSNHL [3].
Carbogen inhalation therapy improves oxygenation and SGB affects vasodilation in the inner ear [1]. The pharmacobiological action of PGE1 includes inhibition of platelet aggregation, cytoprotection, and vasodilatation [4].
Based on this mechanism, PGE1 is used clinically to treat diseases including ISSNHL. In this study, combined therapy of lipo-PGE1 and standard treatment methods were applied to investigate the additional therapeutic effects of lipo-PGE1 on ISSNHL in comparison to other treatment modalities.
We reviewed the medical records of 1,052 patients (539 males and 513 females) diagnosed and treated for ISSNHL from January 1996 to December 2013 (Table 1). Patient ages were 6 to 89 years (Table 1). Patients were divided into four treatment groups. The CP group (steroid, carbogen inhalation, and PGE1 injection; 288 patients) was treated with steroid, carbogen inhalation, and lipo-PGE1. The CS group (steroid, carbogen inhalation, and stellate ganglion block; 232 patients) was treated with steroid, carbogen inhalation, and SGB. The C group (steroid and carbogen inhalation; 284 patients) was treated with steroid and carbogen inhalation. The control group (248 patients) was treated with steroid only.
We evaluated and analyzed therapeutic effects according to factors that influenced recovery. Influencing factors were age, degree of hearing loss, time of initial treatment, association of vertigo or tinnitus, and shape of initial audiogram. We recommended 7 days of admission and bed rest for all patients. All patients received steroid therapy, whether or not it was associated with carbogen inhalation, SGB, and lipo-PGE1. Steroid therapy was intravenous (IV) dexamethasone 20 mg twice a day for 4 days and then 10 mg twice a day for 2 days with a tapering dose for 4 days. Patients receiving steroids also received IV low-molecular dextran, and oral and IV ginkgo biloba extract. Dosage for children was by body weight. CP group patients were selected for lipo-PGE1 treatment according to their preference. The CP group received daily IV infusions of 10 ┬Ąl lipo-PGE1 during admission. Carbogen inhalation therapy consisted of inhalation of a gas mixture 3 times daily for 30 minutes during admission. SGB was administered once daily during admission by an anesthesiologist. Pure tone audiograms were taken daily during hospitalization and during subsequent retest visits. Therapeutic effects were evaluated 2 months after treatment using pure tone average. Siegel's criteria for hearing improvement were used for this study (Table 2). Patients were divided into 4 categories according to final hearing results by Siegel's criteria. For statistical analysis, improvement in hearing results was defined as type I, II, and III by Siegel's criteria. No improvement was defined as hearing results classified as type IV.
Patients were divided into 5 degrees of hearing loss according to level of initial hearing loss: mild (below 40 dB), moderate (41-55 dB), moderate severe (56-70 dB), severe (71-90 dB), and profound (above 91 dB). The shape of initial audiograms was classified into 4 types: flat, ascending, descending, and profound. Statistically significant differences were determined using the Žć2 test (p<0.05). All statistical analyses were performed using SPSS Software (PASW for Windows Rel.18.0.0. 2009; SPSS Inc., Chicago, IL, USA).
Overall hearing improvement was 52.2%, with 549 of 1,052 patients recovering completely. Specific hearing improvements by group were: 195 patients out of 288 (67.7%) in the CP group, 126 of 232 (54.3%) in the CS group, 148 of 284 (52.1%) in the C group, and 80 of 248 (32.2%) in the control group. The total recovery rate of the CP group was higher than the CS, C, and control groups with a significant difference detected (p<0.05) (Fig. 1).
Generally, patients younger than age 50 showed better improvement than patients older than 50, and the difference was significant. For patients younger than 50 years, hearing improvement rates were higher in the CP group than the CS, C, and control groups and the difference was significant (p<0.05) (Table 3). Patients older than 50 showed no significant differences among groups (p>0.05).
Based on initial hearing loss, the total hearing improvement of the CP group was higher than others. The recovery rate of the CP group with less than 90 dB was higher than the rate in the CS, C, and control groups and the difference was significant (p<0.05) (Table 3).
By initial treatment within 1 week from onset, the recovery rate of the CP group was higher than the CS, S, and control groups and the difference was significant (p<0.05). For patients who received initial treatment after 2 weeks from onset, improvement was not seen and no significant differences were detected among groups (p>0.05) (Table 3).
For symptoms associated with ISSNHL, 853 patients (81.1%) complained of tinnitus and 337 (32.0%) had vertigo. Hearing improvement was observed for 440 of 853 patients (51.6%) with tinnitus and 112 of 199 patients (56.3%) with no tinnitus, but the difference was not significant (p>0.05). For patients with tinnitus, the CP group had more hearing improvement than the CS, S, and control groups and the difference was significant (p<0.05). Patients without tinnitus showed no significant differences among groups (p>0.05). Patients with vertigo who had hearing improvement were 116 of 337 (34.4%); patients with no vertigo who had hearing improvement were 429 of 715 (60.0%) and the difference was significant (p<0.05). For patients with vertigo, the CP group had significantly more hearing improvement than the control group. The CP group showed more hearing improvement than the CS, C, and control groups in patients without vertigo with a significant difference (p<0.05) (Table 3).
By initial audiogram shape, 325 patients (30.9%) had a flat type, 246 (23.4%) had an ascending type, 278 (26.4%) had a descending type, and 203 patients (19.3%) had a profound type. The CP group showed more hearing improvement than the control group among patients with flat type audiograms, more hearing improvement the CS, C, and control groups in ascending type, more hearing improvement than the control and C groups in descending type, and more hearing improvement than the control and CS groups in profound type. These differences were all significant (p<0.05) (Table 3).
ISSNHL is defined as a rapid sensorineural hearing loss of over 30 dB or more in at least three continuous frequencies that occurs within 3 days or less with no certain causes [56]. The etiology of ISSNHL is unknown however multifactorial causes including vascular compromise, immunologic diseases, disruption of cochlear membrane, viral infection, trauma, otological tumors, toxicity, neurologic, and metabolic causes are suggested [78]. Although ISSNHL is mainly idiopathic, potential causes should be considered. Vascular and viral mechanisms have been considered as main causes and pathophysiologies of ISSNHL. The vascular theory is commonly accepted, but controversial. The circulatory disturbance theory is related to circulation and oxygenation of the inner ear. Viral etiology has also been reported [6]. A careful and through review of patient history is important because it may provide information on possible causes. The characteristics and onset of hearing loss and symptoms such as vertigo, imbalance, tinnitus, and aural pressure should be identified. Physical and neuro-otological examination should be performed with routine otoscopy and audiometry. Systemic illness should be evaluated if needed. Serological and immunological tests, electronystagmography, and magnetic resonance imaging may also be helpful.
ISSNHL prognosis is influenced by age, gender, time interval between onset and initial treatment, shape of initial audiogram, severity of hearing loss, and associated otological symptoms (vertigo, tinnitus). Poor prognostic factors are more severe hearing loss, flat or high frequency hearing loss, vertigo, childhood age, and age older than 60 [9]. Mattox and Lyles [10] recognized that initial audiogram shape is related to recovery and patients with a low-frequency or mid-frequency (U-shaped) audiogram contour have improved recovery. Recovery prognosis is best when patients are treated early, begin to improve within 2 weeks, and have mild hearing loss with an upward-sloping audiogram and no vertigo. Prognosis is worse for patients who do not improve within 2 weeks and have severe hearing loss with a downward-sloping audiogram and vertigo [11]. Patients without vestibular symptoms tend to have better improvement than patients with vestibular symptoms.
Our study found no significant relationship between audiogram shape, tinnitus, and hearing recovery. We observed that patients who visited the clinic early after onset of hearing loss had better improvement, and the severity of initial hearing loss was also related to hearing improvement. Successful treatment modalities suggested for ISSNHL include steroids, vasodilators, carbogen inhalation, SGB, antiviral agents, prostaglandin E1, dextran, and hyperbaric oxygen [6]. Patients with ISSNHL are usually treated by more than one method. Treatment is mainly based on circulatory disturbance and inflammatory reaction etiology to improve blood circulation or oxygenation of the inner ear [612].
Corticosteroids are the main drugs that are generally used to treat ISSNHL [1314]. The action of steroids is uncertain, but they can be beneficial for infectious, inflammatory, and immune-mediated diseases [6]. Corticosteroids might cause anti-inflammatory and metabolic effects, and alter the immune response [15]. With prolonged use of systemic steroids, significant adverse reactions such as abnormal liver function, gastrointestinal trouble, avascular necrosis, epistaxis, acne, and gluteal abscess can occur [916].
The intratympanic injection of steroids is suggested as a treatment modality for ISSNHL that has two theoretical advantages. One is to increase the local concentration of steroids at the inner ear because of direct steroid uptake through the round window. The other is to decrease the adverse effects of systemic steroids from direct steroid injection to the middle ear [917]. Intratympanic steroid therapy is applied primarily to Meniere's disease, but has been recently been evaluated for treatment of sudden sensorineural hearing loss, tinnitus, and autoimmune ear disease [15]. Various effects of intratympanic steroid injection are reported. Parnes, et al. [18] and Chandrasekhar [9] reported successful results for ISSNHL treated with intratympanic steroid therapy. Antiviral treatment for ISSNHL has been also proposed, according to increasing histological and epidemiological evidence supporting a viral etiology [3]. ISSNHL patients occasionally experience viral upper respiratory infections before hearing loss [10]. Seroconversion to viruses such as influenza B, rubeola, mumps, cytomegalovirus, and varicella zoster has also been reported [37]. Hughes, et al. [19] proposed acyclovir and interferon as possible treatments for ISSNHL [20]. Carbogen inhalation therapy, in which patients breathe a gas mixture of 5% carbon dioxide (CO2) and 95% oxygen (O2), is applied to improve peripheral tissue perfusion and oxygenation of the inner ear to treat ISSNHL. Fisch, et al. [21] reported increased O2 tension in the perilymph in humans and Kallinen, et al. [12] reported a change in cochlear blood flow (CBF) in guinea pigs after inhalation of a carbogen gas mixture. SGB induces vasodilatation by blocking postganglionic sympathetic fibers in inner ear vessels originating from the stellate ganglion [6]. Haug, et al. [22] reported using SGB to treat patients with ISSNHL. PGE1 is a vasodilator and potent inhibitor of platelet aggregation and has been used to treat several vascular diseases and ISSNHL [23]. Since PGE1 is rapidly metabolized in the lungs, IV treatment requires large doses, making PGE1 difficult to use clinically and increasing systemic adverse effects such as arrhythmia, venous thrombosis, and thrombophlebitis. PGE1 can be coated with a 0.2 ┬Ąg lipid microsphere produced by beans to prevent rapid metabolism. The coating of lipo-PGE1, which is designated to protect PGE1 from being rapidly metabolized, has been used clinically with therapeutic effects at small doses with fewer side effects [24]. The vasodilating action of PGE1 is thought to be endothelium independent. PGE1 receptors are found on vascular smooth muscle cell membranes. When PGE1 binds to receptors, stimulatory G proteins activate adenyl cyclase to generate cyclic monophosphate (cAMP), which relaxes smooth muscle for vasodilatation [25]. Vasodilators increase cardiac output and systemic blood flow and increase oxygen delivery by improving CBF. Because the decreased systemic blood pressure (SBP) induced by PGE1 is caused by systemic vasodilation, systemic circulatory volume may remain unchanged. Therefore, alteration of CBF may depend on drug selectivity in the ear. Nishimura, et al. [24] suggested that both PGE1 and lipo-PGE1 resulted in a dose-dependent decrease in SBP and maintenance of CBF in spite of decreased SBP. However, no significant increase in CBF is observed with either drug. In comparing the effects of PGE1 and lipo-PGE1, no differences in the effects on SBP and CBF are observed [25].
PGE1 inhibits platelet aggregation, which is effective at improving cochlear vascular circulatory disorders. An increase in cellular cAMP decreases platelet Ca2+ and relaxes contracted platelet aggregates. PGE1 activation results in secretion of CIŌłÆ ions, which induces Na+ and K+ extrusion via a pump, leading to decreased platelet volume. Therefore, PGE1 therapy may be effective for the ears of patients with vascular circulatory disorders [26]. Ahn, et al. [4] reported that a lipo-PGE1-treated group showed hearing improvement that was not statistically significant. Nakashima, et al. [27] found PGE1 had no beneficial effect on ISSNHL. Ogawa, et al. [28] reported that PGE1 had a significant effect on hearing gain at high frequency in patients with severe tinnitus. In our study, a significant difference was observed in hearing improvement between patients treated with lipo-PGE1 and other modalities. Early treatment and hospitalization are required for patients with ISSNHL, and the prognosis is not good when patients fail to recover within 2 weeks after treatment initiation. In our study, we observed hearing improvement after 1 month of treatment more often in the lipo-PGE1 group than other treatment groups. We expect to find more effective therapeutic results at long-term follow-up for ISSNHL treated with lipo-PGE1. Our preliminary results on treating ISSNHL with lipo-PGE1 seem promising. We propose that combined lipo-PGE1 treatment is a relatively more effective therapy compared to standard treatment. Further studies with larger series may be required to statistically verify results for patients treated by lipo-PGE1 for ISSNHL.
In conclusion, multiple drug regimens are considered more effective for treating ISSNHL which might have several different etiologies and has no universally accepted treatment. The results of this study showed that combined lipo-PGE1 treatment was more effective than other treatment modalities for ISSNHL. Significant differences in hearing improvement were observed among groups treated with lipo-PGE1 and other groups. The lipo-PGE1 groups had more hearing improvement in patients with initial treatment within 1 week and patients younger than 50. Differences from comparison groups were significant. Improvement in hearing was worse in patients with profound initial hearing loss. Initial audiogram shape was not predictive of improvement. A significant trend was seen for better hearing results in patients without vertigo.
References
1. Kallinen J, Kuttila K, Aitasalo K, Gr├®nman R. Effect of carbogen inhalation on peripheral tissue perfusion and oxygenation in patients suffering from sudden hearing loss. Ann Otol Rhinol Laryngol 1999;108:944ŌĆō947. PMID: 10526848.

2. Choung YH, Park K, Shin YR, Cho MJ. Intratympanic dexamethasone injection for refractory sudden sensorineural hearing loss. Laryngoscope 2006;116:747ŌĆō752. PMID: 16652082.

3. Fetterman BL, Saunders JE, Luxford WM. Prognosis and treatment of sudden sensorineural hearing loss. Am J Otol 1996;17:529ŌĆō536. PMID: 8841697.
4. Ahn JH, Kim MR, Kim HC. Therapeutic effect of lipoprostaglandin E1 on sudden hearing loss. Am J Otolaryngol 2005;26:245ŌĆō248. PMID: 15991090.

5. Gianoli GJ, Li JC. Transtympanic steroids for treatment of sudden hearing loss. Otolaryngol Head Neck Surg 2001;125:142ŌĆō146. PMID: 11555744.

6. Haberkamp TJ, Tanyeri HM. Management of idiopathic sudden sensorineural hearing loss. Am J Otol 1999;20:587ŌĆō592. discussion 593-5. PMID: 10503580.

7. Wilson WR, Veltri RW, Laird N, Sprinkle PM. Viral and epidemiologic studies of idiopathic sudden hearing loss. Otolaryngol Head Neck Surg 1983;91:653ŌĆō658. PMID: 6420747.

8. Lee JW, Park YA, Park SM, Kong TH, Park SY, Bong JP, et al. Clinical features and prognosis of sudden sensorineural hearing loss secondary to intralabyrinthine hemorrhage. J Audiol Otol 2016;20:31ŌĆō35. PMID: 27144231.



9. Chandrasekhar SS. Intratympanic dexamethasone for sudden sensorineural hearing loss: clinical and laboratory evaluation. Otol Neurotol 2001;22:18ŌĆō23. PMID: 11314710.

10. Mattox DE, Lyles CA. Idiopathic sudden sensorineural hearing loss. Am J Otol 1989;10:242ŌĆō247. PMID: 2665512.
11. Mattox DE, Simmons FB. Natural history of sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol 1977;86(4 Pt 1):463ŌĆō480. PMID: 889223.

12. Kallinen J, Laurikainen E, Laippala P, Gr├®nman R. Sudden deafness: a comparison of anticoagulant therapy and carbogen inhalation therapy. Ann Otol Rhinol Laryngol 1997;106:22ŌĆō26. PMID: 9006356.

13. Roh KJ, Lee EJ, Park AY, Choi BI, Son EJ. Long-term outcomes of acute low-tone hearing loss. J Audiol Otol 2015;19:74ŌĆō78. PMID: 26413572.



14. Chang J, Yum G, Im HY, Jung JY, Rah YC, Choi J. Short-term outcomes of acute low-tone sensorineural hearing loss according to treatment modality. J Audiol Otol 2016;20:47ŌĆō52. PMID: 27144234.



15. Doyle KJ, Bauch C, Battista R, Beatty C, Hughes GB, Mason J, et al. Intratympanic steroid treatment: a review. Otol Neurotol 2004;25:1034ŌĆō1039. PMID: 15547441.

16. Alexiou C, Arnold W, Fauser C, Schratzenstaller B, Gloddek B, Fuhrmann S, et al. Sudden sensorineural hearing loss: does application of glucocorticoids make sense? Arch Otolaryngol Head Neck Surg 2001;127:253ŌĆō258. PMID: 11255468.

17. Goycoolea MV, Muchow D, Schachern P. Experimental studies on round window structure: function and permeability. Laryngoscope 1988;98(6 Pt 2):Suppl 44. 1ŌĆō20.

18. Parnes LS, Sun AH, Freeman DJ. Corticosteroid pharmacokinetics in the inner ear fluids: an animal study followed by clinical application. Laryngoscope 1999;109(7 Pt 2):1ŌĆō17.

19. Hughes GB, Freedman MA, Haberkamp TJ, Guay ME. Sudden sensorineural hearing loss. Otolaryngol Clin North Am 1996;29:393ŌĆō405. PMID: 8743339.

20. Khetarpal U, Nadol JB Jr, Glynn RJ. Idiopathic sudden sensorineural hearing loss and postnatal viral labyrinthitis: a statistical comparison of temporal bone findings. Ann Otol Rhinol Laryngol 1990;99:969ŌĆō976. PMID: 2244729.

21. Fisch U, Murata K, Hossli G. Measurement of oxygen tension in human perilymph. Acta Otolaryngol 1976;81:278ŌĆō282. PMID: 1266613.

22. Haug O, Draper WL, Haug SA. Stellate ganglion blocks for idiopathic sensorineural hearing loss. Arch Otolaryngol 1976;102:5ŌĆō8. PMID: 1244832.

23. Clifford PC, Martin MF, Sheddon EJ, Kirby JD, Baird RN, Dieppe PA. Treatment of vasospastic disease with prostaglandin E1. Treatment of vasospastic disease with prostaglandin E1. Br Med J 1980;281:1031ŌĆō1034. PMID: 7427564.
24. Nishimura T, Nario K, Hosoi H. Effects of intravenous administration of prostaglandin E(1) and lipo-prostaglandin E(1) on cochlear blood flow in guinea pigs. Eur Arch Otorhinolaryngol 2002;259:253ŌĆō256. PMID: 12107528.

25. Murray KJ. Cyclic AMP and mechanisms of vasodilation. Pharmacol Ther 1990;47:329ŌĆō345. PMID: 1963221.

26. Salganicoff L, Russo MA. An hypothesis on the consolidation and PGE1-induced deconsolidation of a platelet plug. Platelets 2003;14:463ŌĆō471. PMID: 14713515.

27. Nakashima T, Kuno K, Yanagita N. Evaluation of prostaglandin E1 therapy for sudden deafness. Laryngoscope 1989;99:542ŌĆō546. PMID: 2709943.

28. Ogawa K, Takei S, Inoue Y, Kanzaki J. Effect of prostaglandin E1 on idiopathic sudden sensorineural hearing loss: a double-blinded clinical study. Otol Neurotol 2002;23:665ŌĆō668. PMID: 12218617.

Fig.┬Ā1
*p<0.05: CP vs. control, ŌĆĀp<0.05: CP vs. C, ŌĆĪp<0.05: CP vs. CS.Control: medication only, C: medication and carbogen inhalation, CS: medication, carbogen inhalation, and stellate ganglion block, CP: medication, carbogen inhalation, and PGE1 injection.
Table┬Ā1.
Patients demographics
Table┬Ā2.
Siegel's criteria (1985)
Table┬Ā3.
Comparison of recovery rates according to variables (%)
| Control | C group | CS group | CP group | Total | |
|---|---|---|---|---|---|
| Age | |||||
| ŌĆāUnder 20 | 22.2 | 67.7 | 85.7 | 79.3 | 65.2 |
| ŌĆā20-29 | 35.0 | 73.7 | 69.0 | 82.1 | 61.2 |
| ŌĆā30-39 | 18.5 | 65.2 | 60.3 | 80.4 | 55.0 |
| ŌĆā40-49 | 48.1 | 54.5 | 59.1 | 78.3 | 60.6 |
| ŌĆā50-59 | 30.4 | 41.3 | 36.1 | 43.5 | 38.6 |
| ŌĆāAbove 60 | 33.3 | 37.1 | 41.3 | 57.1 | 43.3 |
| Initial hearing loss level | |||||
| ŌĆāBelow 40 dB | 50.0 | 36.7 | 60.0 | 60.0 | 48.9 |
| ŌĆā41-55 dB | 35.0 | 43.9 | 61.9 | 81.6 | 55.3 |
| ŌĆā56-70 dB | 33.3 | 50.0 | 55.2 | 73.8 | 53.7 |
| ŌĆā71-90 dB | 37.5 | 62.5 | 60.4 | 75.0 | 60.6 |
| ŌĆāAbove 90 dB | 24.4 | 45.8 | 33.3 | 53.7 | 40.1 |
| Beginning of treatment | |||||
| ŌĆā-1 week | 34.5* | 54.9ŌĆĀ | 59.5ŌĆĪ | 72.4 | 58.5 |
| ŌĆā1-2weeks | 14.3 | 50.0 | 45.5 | 45.8 | 45.7 |
| ŌĆā2 weeks- | 14.3 | 23.5 | 25.0 | 25.0 | 21.9 |
| Tinnitus | |||||
| ŌĆāWith | 25.5* | 52.6ŌĆĀ | 56.3ŌĆĪ | 68.6 | 51.6 |
| ŌĆāWithout | 57.7 | 50.0 | 48.6 | 66.1 | 56.3 |
| Vertigo | |||||
| ŌĆāWith | 16.1* | 37.3 | 47.6 | 52.2 | 34.4 |
| ŌĆāWithout | 48.4* | 58.7ŌĆĀ | 54.4ŌĆĪ | 71.9 | 60.0 |
| Initial audiogram | |||||
| ŌĆāFlat | 41.7* | 58.7 | 65.2 | 67.2 | 62.1 |
| ŌĆāAscending | 55.3* | 62.2ŌĆĀ | 50.0ŌĆĪ | 82.1 | 63.9 |
| ŌĆāDescending | 13.8* | 49.5ŌĆĀ | 68.7 | 69.4 | 55.4 |
| ŌĆāProfound | 15.2* | 37.5 | 21.1ŌĆĪ | 45.2 | 31.8 |
- TOOLS






