Is Ossiculoplasty Necessary in Canal Wall Down Mastoidectomy? Comparison of Clinical Outcomes Between Type 0 Tympanoplasty and Ossiculoplasty
Article information
Abstract
Background and Objectives
To assess whether the audiological and clinical outcomes of type 0 tympanoplasty (T0) performed using cartilage were comparable with those of ossiculoplasty in patients who underwent canal wall down mastoidectomy (CWDM).
Subjects and Methods
This study included patients who had chronic otitis media with cholesteatoma and underwent CWDM with ossiculoplasty involving partial ossicular replacement prosthesis (PORP), total ossicular replacement prosthesis (TORP), or T0. Anatomical success rates and hearing outcomes were analyzed.
Results
Seventy-two patients were included in this study; 29 of them underwent CWDM with T0, 27 underwent CWDM with PORP, while 16 underwent CWDM with TORP. The difference in mean improvement in the air-bone gap (ABG) between the groups was not significant. The differences in the rates of ABG closure to ≤10 dB HL (p=0.030) and ≤20 dB HL (p=0.029) were significant. There were significant differences in improvements in the ABG at 3 kHz among the PORP, TORP, and T0 groups.
Conclusions
The audiological outcomes of CWDM with ossiculoplasty seemed to be better than those of CWDM with T0 with no significant difference in the incidence of complications following ossiculoplasty and T0.
Introduction
Eradication of lesions is the most important purpose of mastoidectomy for chronic otitis media (COM) with or without cholesteatoma. Conventionally, canal wall down mastoidectomy (CWDM) is considered the gold standard for a dry and safe ear [1]. Satisfactory functional results are required in these patients. In many cases, to improve hearing, ossiculoplasty (i.e., repair of an intact ossicular chain) is performed after CWDM or simultaneously.
When planning for staged ossiculoplasty or when there is a high expectation of recurrence because of poor Eustachiantube function, ossiculoplasty is not performed with CWDM in cases of ossicular disruption. Instead, patients undergo CWDM with type 0 tympanoplasty (T0), wherein a graft is placed without the intention of restoring hearing or connecting the graft and the ossicles. Immediately after the operation, there is no connection between the tympanoplasty graft and ossicles. This is determined by a substantial air-bone gap (ABG) in the pure-tone audiometry test. However, hearing test results improve in some of these patients. Several months after CWDM with T0, the graft might retract because of poor Eustachian tube function, and the graft might connect to the ossicles, which would result in the restoration of sound conduction. These experiences led the authors to question whether ossiculoplasty should be performed when patients undergo CWDM.
The aim of this study was to assess whether the audiological and clinical outcomes of T0 using cartilage were comparable to those of ossiculoplasty including a partial ossicular replacement prosthesis (PORP) and total ossicular replacement prosthesis (TORP) in patients with COM who underwent CWDM.
Subjects and Methods
Subjects
The medical records of patients who underwent CWDM at a secondary hospital between March 2013 and October 2017 were retrospectively reviewed. This study included adults over 19 years who had chronic otomastoiditis with middle ear cholesteatoma confirmed by computed tomography (CT) and underwent CWDM with T0 or ossiculoplasty in a single-stage surgery. Patients with perforation that involved over 50% of the tympanic membrane (TM) were enrolled in this study. Revision surgeries were also performed. The revision cases in this study only involved a history of tympanoplasty without mastoidectomy or canal wall up mastoidectomy (CWUM) with tympanoplasty. No patient showed an inner ear anomaly on a CT. Patients with a bone conduction (BC) hearing threshold of >65 dB HL preoperatively were excluded from this study. Patient demographics, surgical complications, and clinical and audiological outcomes were evaluated. Patients were divided according to surgical procedure: those who underwent CWDM with T0, ossiculoplasty using a PORP, and ossiculoplasty using a TORP.
Surgical technique
All surgeries were performed by three surgeons. Ossiculoplasty was performed by two surgeons using a PORP or TORP according to the presence or absence of the stapes suprastructure in a single-stage surgery with CWDM. Titanium ossicular replacement prostheses were used for all ossiculoplasties. The other surgeon performed T0 using cartilage in all CWDM surgeries for COM with cholesteatoma. Patients who underwent CWDM with T0 using cartilage had an intact and mobile stapes, but the incus or malleus was eroded by disease or removed by a surgeon to obtain better surgical results. The modified palisade technique was used for cartilage reconstruction of the TM. Cartilage was cut into several slices that were subsequently pieced together, like the pieces of a mosaic tile or a jigsaw puzzle, to reconstruct the TM. Cartilage from the cavum area was used in this study, instead of cymbal or tragal cartilage, which was used in a previous study [2].
Analysis of surgical results and audiological tests
We examined the status of the TM after surgery using an endoscope and microscope. Any complications were noted, including postoperative dizziness, facial palsy, re-perforation of the TM, wound infection including myringitis, and extrusion of the prosthesis.
We also performed pure-tone audiometry to evaluate the patients’ hearing abilities. The pure-tone average was calculated according to the four-frequency average method [(0.5 kHz+1 kHz+2 kHz+4 kHz)/4]. Pure-tone thresholds for air conduction (AC) and BC were noted pre- and post-operatively, and the ABG was calculated. If a patient underwent pure-tone audiometry several times after surgery, the result from the last follow-up visit was used.
Statistical analysis
The differences in hearing performance between the groups were compared using the linear-by-linear association test, Wilcoxon signed-rank test, Mann-Whitney U test, and Kruskal-Wallis test (IBM SPSS statistics 23, IBM Corp., Armonk, NY, USA). Statistical significance was set at p<0.05.
Ethics committee approval and informed consent
This retrospective study was conducted under the review and approval of the Institutional Review Board of a secondary hospital (IRB No. JEJUNUH 2018-08-002), and the requirement for informed consent from each patient was waived.
Results
Seventy-two patients (32 male and 40 female, mean age=53.4 years) were eligible based on our inclusion criteria. The mean follow-up period was 22.1 months. Twenty-nine patients underwent CWDM with T0, 27 underwent CWDM with PORP, and 16 underwent CWDM with TORP. The demographic characteristics of the 72 patients, including age at CWDM, duration of follow-up, and diagnosis are shown in Table 1.
The average ABG decreased from 27.5±12.2 dB HL preoperatively to 24.4±14.1 dB HL postoperatively in the T0 group. In the PORP group, the average ABG decreased from 20.5±10.0 dB HL preoperatively to 13.6±11.5 dB HL postoperatively, it decreased from 16.3±13.3 dB HL preoperatively to 13.4±12.0 dB HL postoperatively in the TORP group. Mean improvements in the ABG of 3.1±14.6 dB HL, 6.9±13.1 dB HL, and 2.9±8.3 dB HLwere noted in the T0, PORP, and TORP group, respectively (Table 2). The difference in mean improvement in the ABG between the groups was not statistically significant (p=0.211).
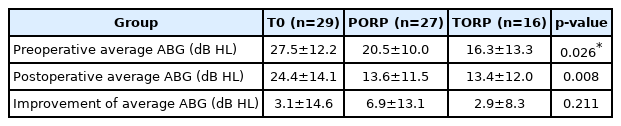
Comparison of pre and postoperative average ABG and improvement of average ABG between T0 and ossiculoplasty groups
The mean thresholds of BC increased 3.6, 3.8, 7.1, 9.3, and 11.6 dB HL at 0.5, 1, 2, 3, and 4 kHz in the T0 group, and by 13.7, 13.1, 9.6, 13.9, and 17 dB HL in the PORP group, respectively. In the TORP group, the mean BC thresholds increased by 2.8 and 3.4 dB HL at 3 and 4 kHz respectively, but they decreased by 3.8, 3.8, and 1.3 dB HL at 0.5, 1, and 2 kHz, respectively. At 0.5, 1, 2, 3, and 4 kHz, the mean thresholds of AC increased by 3.3, 0.3, 1.4, 4.7, and 9dB HL in the T0 group; by 5.4, 3.1, 4.3, 1.3, and 1.3 dB HL in the PORP group; and by 5.9, 6.6, 1.9, 0.6, and 2.8 dB HL in the TORP group, respectively. At 0.5, 1, 2, 3, and 4 kHz, the mean ABG decreased by 0.3, 3.4, 5.7, 4.7, and 2.6 dB HL in the T0 group; by 8.3, 10.0, 5.3, 12.6, and 12.0 dB HL in the PORP group; and by 2.2, 2.8, 0.6, 3.4, and 6.3 dB HL in the TORP group, respectively. The detailed audiologic results of the groups at 0.5, 1, 2, 3, and 4 kHz were shown at Table 3. In many cases, the BC threshold worsened after CWDM surgery. However, compared to the degree of worsening of the BC threshold, the degree of worsening of the AC threshold was relatively low, and the mean ABG improved at every frequency.

Pre and postoperative improvement of BC, AC, and ABG at 0.5, 1, 2, 3, and 4 kHz between T0 and ossiculoplasty groups
The rates of ABG closure to ≤10, ≤20, and ≤30 dB HL are depicted in Fig. 1. The differences in the rates of ABG closure to ≤10 dB HL (p=0.030) and ≤20 dB HL (p=0.029) were statistically significant.

Rates of ABG closure to ≤10, ≤20, and ≤30 dB HL. The percentages of patients in the T0, PORP, and TORP groups showing ABG closure to ≤10 dB HL were 17.2%, 33.3%, and 43.8%, respectively. The percentages of patients in the corresponding groups showing ABG closure to ≤20 dB HL were 34.5%, 55.6%, and 68.8%, respectively. The percentages of patients in the corresponding groups showing ABG closure to ≤30 dB HL were 62.1%, 77.8%, and 87.5%, respectively. *p<0.05. ABG: air-bone gap, T0: type 0 tympanoplasty, PORP: partial ossicular replacement prosthesis, TORP: total ossicular replacement prosthesis.
One patient showed re-perforation, while two patients had prosthesis extrusion, which required additional surgical intervention. Delayed facial palsy was observed in two patients and was resolved by conservative management. Infections related to surgery were identified in two patients, and temporary dizziness was observed in three patients. No recurrence of cholesteatoma was found during the follow-up period (Table 4).
Discussion
Although some studies have reported similar audiological results on comparing CWUM and CWDM [3,4], an intact posterior canal wall was assessed as a positive prognostic factor for hearing outcomes in other reports [5-7]. After removing the disease in the middle ear and mastoid cavity using the CWDM technique, procedures to restore sound conduction should be considered.
A variety of methods and materials have been used to restore sound transmission, including incus transposition [8], use of hydroxyapatite or titanium ossicular replacement prosthesis [9], and use of autologous or homologous cartilage grafts [10,11]. Although no material has been clearly demonstrated to yield better results than the others [9,12], a manufactured PORP and TORP are popular options for repairing the ossicular chain. Complications related to ossiculoplasty include the need for subsequent surgery, secondary ventilation tube insertion, displacement of the prosthesis, extensive scar tissue formation, and recurrence of perforation [13]. Tympanoplasty without ossiculoplasty may reduce complications and additional costs.
Some patients with an intact stapes attained better hearing without additional ossiculoplasty after T0 (Fig. 2). A possible reason is that due to poor Eustachian tube ventilation, the T0 graft is gradually retracted after the first surgery and connected to the stapes head resulting in a type III cartilage tympanoplasty. In a study on the treatment of cholesteatoma using CWUM, when the stapes is preserved, cartilage tympanoplasty on the stapes head yielded acceptable functional results similar to those obtained with the use of a PORP. With a follow-up of two years, the residual mean ABG was 16.8 dB HL in the group treated with cartilage tympanoplasty over the stapes head and 15.8 dB HL in the hydroxyapatite PORP group. The ABG was <20 dB HL in 67.6% of cases in the cartilage tympanoplasty group and 70.4% of cases in the hydroxyapatite PORP group. No significant differences were observed between the two techniques [14].
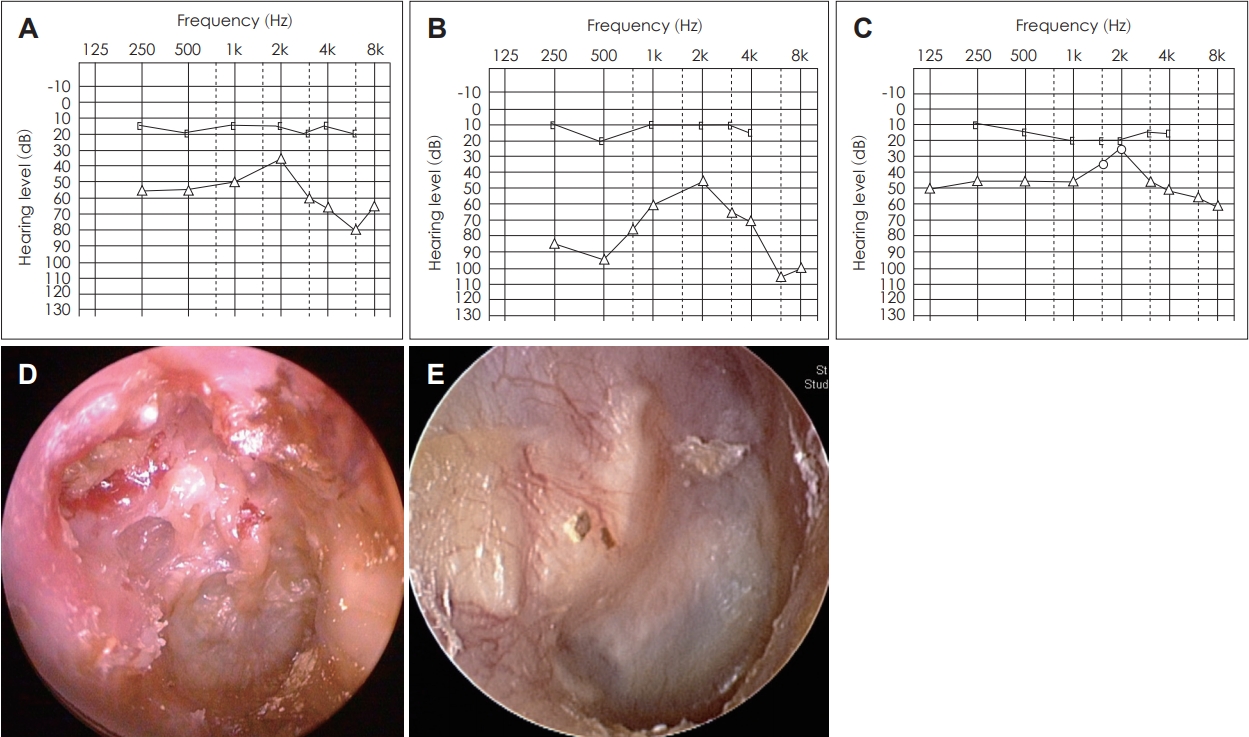
Audiological and anatomical results of CWDM with T0 in the right ear. A: Preoperative pure-tone audiometry shows that the patient had an ABG. B: It became worse 3 months after surgery. C: The hearing test result improved 6 months after surgery. D: Attic destruction is observed on the preoperative otoscopic examination. E: Postoperative findings of the tympanic membrane after CWDM with T0. CWDM: canal wall down mastoidectomy, ABG: air-bone gap, T0: type 0 tympanoplasty.
However, ossiculoplasty between the TM and the stapes or its footplate was associated with better hearing gain than tympanoplasty alone in a study that evaluated functional results in groups of patients with homogeneous disease severity who underwent CWDM. They reported a mean ABG of 24.06 dB HL in ossiculoplasty group and 35.54 dB HL in the type III/IV tympanoplasty group [15].
While the differences in audiological outcomes were not significant between the PORP, TORP, and T0 groups with respect to most variables, the audiological results in the T0 group seemed to be worse than those in the ossiculoplasty groups in this study. Furthermore, the differences in the rates of ABG closure to ≤10 dB HL and ≤20 dB HL and the improvement in the ABG in 3 and 4 kHz were statistically significant.
The limitations of this study include its small sample size, short follow-up period, and variability in COM status. The size of the TM perforation and the condition of the ossicles were not identical, and therefore, the preoperative and postoperative average ABGs showed significant differences in each group. In addition, surgeries were performed by different surgeons, which may introduce a bias. Some patients experienced deterioration of BC thresholds after surgery. Surgical treatment of chronic middle ear disease can affect BC thresholds in numerous ways: damage to the cochlea, including acoustic trauma by drill-generated noise or suction; excessive movement of the ossicles; and damage to the oval window, or lateral semicircular canal during the removal of cholesteatoma or granulations from these sensitive areas. However, the clearance of cholesteatoma, granulations, adhesions, or pus results in the removal of mechanical obstructions from the oval and round windows and can result in improved BC thresholds in a number of cases [16].
Despite these limitations, our study demonstrates that the audiological outcomes of CWDM with ossiculoplasty were better than those of CWDM with T0, while the complications following T0 and ossiculoplasty were not significantly different.
Acknowledgements
None
Notes
Conflicts of interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Chan Il Song. Data curation: Jin-A Park, Hee Jun Yi. Formal analysis: Michelle J. Suh. Investigation: Chan Il Song. Methodology: Michelle J. Suh, Jin-A Park. Project administration: Hee Jun Yi, Chan Il Song. Supervision: Chan Il Song. Validation: Chan Il Song. Visualization: Jin-A Park, Hee Jun Yi. Writing— original draft: Michelle J. Suh. Writing—review & editing: Chan Il Song. Approval of final manuscript: all authors.


