 |
 |
- Search
| J Audiol Otol > Volume 27(3); 2023 > Article |
|
Abstract
Notes
Ethics Statement
Written informed consent was obtained from the patients, for publication of these case reports and of the accompanying images.
Author Contributions
Conceptualization: Athanasios Luca Fountarlis, Charalampos Skoulakis. Data curation: Vasileios Lachanas, Ioannis Tsitiridis. Formal analysis: Athanasios Luca Fountarlis, Jiannis Hajiioannou. Methodology: Athanasios Saratziotis, Aggeliki Alagianni. Supervision: Aggeliki Alagianni, Jiannis Hajiioannou, Charalampos Skoulakis. Visualization: Athanasios Luca Fountarlis, Athanasios Saratziotis. Writing— original draft: Athanasios Luca Fountarlis. Writing—review & editing: Jiannis Hajiioannou. Approval of final manuscript: all authors.
Fig. 1.
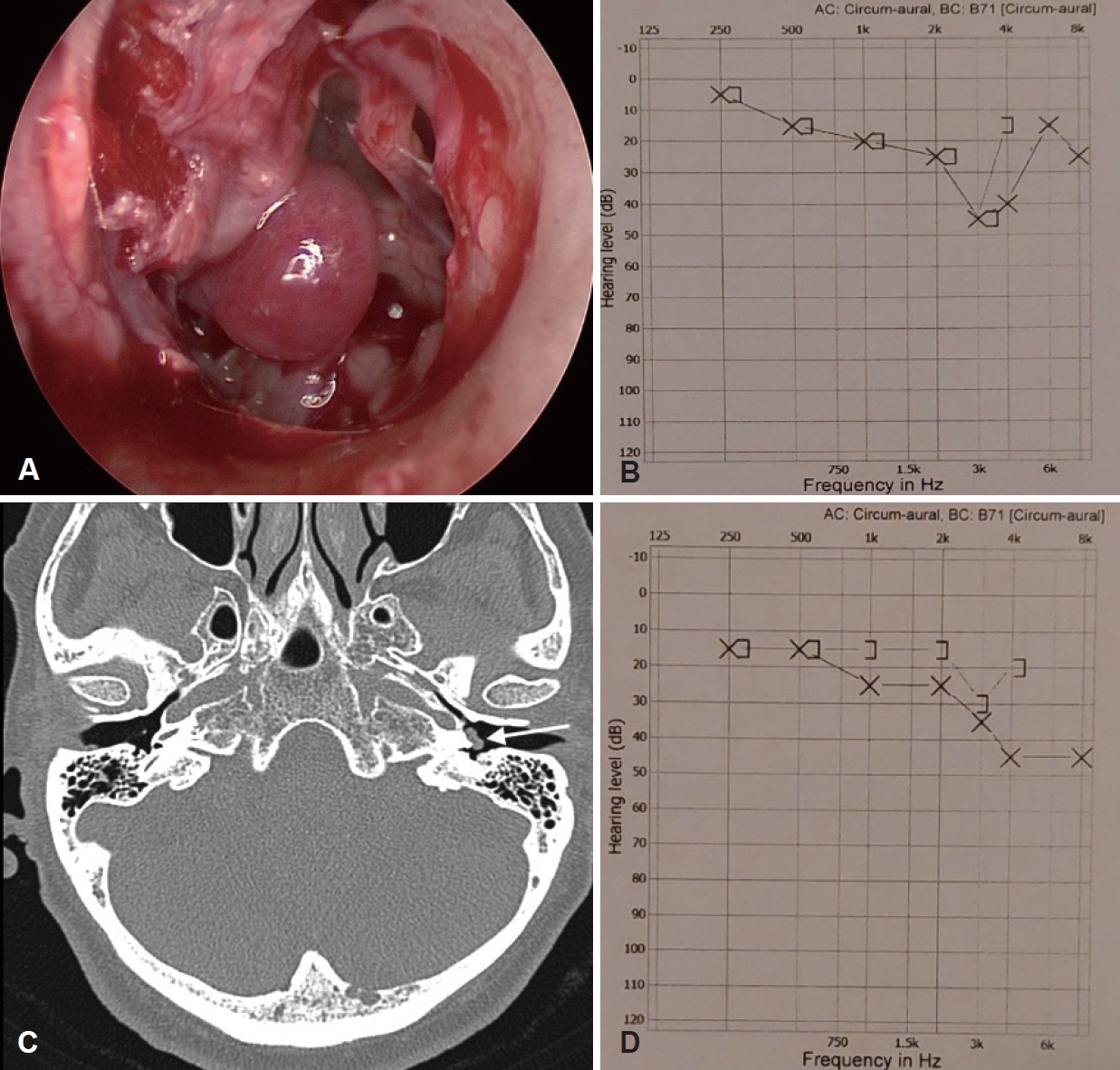
Fig. 2.

Fig. 3.

Table 1.
| Class | Definition |
|---|---|
| Glasscock-Jackson classification [7] | |
| 1 | Tumor completely visible on otoscopy |
| 2 | Tumor completely filling the middle ear cavity |
| 3 | Tumors filling the middle ear cavity and extending into the mastoid |
| 4 | Tumor extending through the tympanic membrane into the external auditory canal |
| Modified Fisch-Mattox classification [6] | |
| A1 | Tumor limited to the middle ear cavity and completely visible on otoscopic examination |
| A2 | Tumor limited to the middle ear cavity but the margins are not visible on otoscopy – may extend to the Eustachian tube and/or to the posterior mesotympanum |
| B1 | Tumor filling the middle ear cavity with extension into the hypotympanum and tympanic sinus |
| B2 | Tumor filling the middle ear cavity, extending into the mastoid and medially to the mastoid segment of the facial nerve |
| B3 | Tumor filling the middle ear cavity, extending into the mastoid with erosion of carotid canal |
Table 2.
Table 3.
| Study | Type of study | Country | No. of patients | Age mean (range)* | F/M | GJ classification | mFM classification |
|---|---|---|---|---|---|---|---|
| Marchioni, et al. [5] | Case series | Italy | 3 | 33, 57, 67 | 2/1 | NA | 1 Α1, 2 Β1 |
| Daneshi, et al. [13] | Case series | Iran | 13 | 54 (44-68) | 9/4 | 6 (I), 7 (II) | NA |
| Pollak and Soni [3] | Case report | USA | 1 | 74 | 1/0 | (I) | A1 |
| O’Connell, et al. [9] | Two case reports | USA | 2 | 53, 64 | 0/2 | 1 (I), 1 (II) | NA |
| Killeen, et al. [1] | Case series | USA, Brazil | 14 | 61.6 (34-82) | 13/1 | 13 (I), 1 (II) | 1 A1, 13 A2 |
| Noel and Sajjadi [12] | Case series | USA | 5 | 57.2 (38-77) | 2/3 | NA | NA |
| Okhi and Kikuchi [8] | Case report | Japan | 1 | 51 | 1/0 | (I) | A1 |
| Teh, et al. [16] | Case report | Malaysia | 1 | 53 | 1/0 | (II) | NA |
| Vicario-Quiñones, et al. [15] | Two case reports | Spain | 2 | 70, 74 | 2/0 | 2 (I) | NA |
| Kaul, et al. [2] | Case series | USA | 8 | NA (43-83) | NA | NA | NA |
| Fermi, et al. [14] | Case series | Italy, Egypt | 30 | 56.6 (22-82) | 25/5 | 14 (I), 16 (II) | 11 A1, 10 A2, 9 B1 |
| Pradhan, et al. [10] | Case report | India | 1 | 50 | 1/0 | NA | NA |
| Quick, et al. [4] | Case series | Australia | 10 | 45.5 (25-69) | 9/1 | 5 (I), 5 (II) | 5 A1, 2 A2, 3 B1 |
| Total | 91 | 66/17 | 43 (I), 31 (II) | 20 A1, 25 A2, 14 B1 |
Table 4.
| Study | Excusive endoscopic approach | Complete removal | Audiologic results | Complications | Operative time (min) | Hemostasis technique | Time of follow-up (mo) mean (range) | Recurrence |
|---|---|---|---|---|---|---|---|---|
| Marchioni, et al. [5] | 3/3 | 3/3 | 1↑ 1↓ 1= | HL | NA | 3 BC, 1 CO2L | 10.7 (5-18) | No |
| Daneshi, et al. [13] | 13/13 | 13/13 | 10↑ 0↓ 3= | None | 60 (45-120) | 9 BC, 4 APC-L | 20 (NA) | No |
| Pollak and Soni [3] | 1/1 | 1/1 | 1= | None | NA | CO2L | 8 | No |
| O’Connell, et al. [9] | 2/2 | 2/2 | 1↑ 1= | None | 52, 96 | NA | None | No |
| Killeen, et al. [1] | 11/14 | 14/14 | 8↑ 3↓ 1= | None | 108.1 (58-248) | KTP-L, diode-L, CO2L, temporary packing | 11.1 (NA) | No |
| Noel and Sajjadi [12] | 4/5 | 5/5 | 5= | None | NA | KTP-L | 23.2 (12-38) | No |
| Okhi and Kikuchi [8] | 1/1 | 1/1 | 1= | NA | 66 | Temporary packing | 36 | No |
| Teh, et al. [16] | 1/1 | 1/1 | 1= | NA | NA | Monopolar suction diathermy | 1 | No |
| Vicario-Quiñones, et al. [15] | 2/2 | 1/1* | 1↓ 1NA | 1 TM perforation | NA | CO2L | 6 | No |
| Kaul, et al. [2] | 8/8 | 8/8 | NA | 1 temporary tinnitus | NA | KTP-L | NA | NA |
| Fermi, et al. [14] | 30/30 | 27/30 | 4↑ 3↓ 13= | 1 TM perforation, 4 dysgeusia | 115.2 (NA) | BC, diamond burr | 38.1 (18-103) | No |
| Pradhan, et al. [10] | 1/1 | 1/1 | NA | TM perforation | 110 | NA | 12 | No |
| Quick et, al. [4] | 10/10 | 10/10 | 1↑ 2↓ 6= | 1 TM perforation | 98 (60-160) | 4 BC, 7 CO2L | 10 (4-25) | No |
| Total | 87/91 | 87/90 |
↑, hearing improvement; ↓, hearing deterioration; =, hearing stable (changes up to 10 dB were considered as hearing stable); HL, hearing loss; TM, tympanic membrane; BC, bipolar cautery; CO2L, CO2 laser; APC-L, argon plasma coagulation laser; KTP-L, potassium titanyl phosphate laser; diode-L, diode laser; NA, not available







