Endoscopic Management of Glomus Tympanicum Tumor: Report of Three Cases and Review of the Literature
Article information
Abstract
Glomus tympanicum are benign tumors of vascular origin, arising from the neural crest cells and located on promontory. The treatment of choice is surgical excision of the lesion. Traditionally, it is performed under microscopic observation. With the introduction of endoscopes in the field of ear surgeries, an endoscopic approach has also evolved. Herein, we present case reports of three patients diagnosed with glomus tympanicum tumors who were operated on using an endoscopic approach. A review of the literature is also performed. The mass was completely excised in all patients, and there were no signs of recurrence at the follow-up at least a year later. Endoscopic ear surgery is a safe and effective method of managing glomus tympanicum tumors. Its main limitation is the tumor size; however, in most cases, tumors of stages I to II as per the Glasscock-Jackson classification and types A1 to B1 according to the modified Fisch-Mattox classification can be completely removed endoscopically. Careful preoperative selection of patients warrants the best outcomes.
Introduction
Glomus tympanicum tumors (GTT), also called middle ear paragangliomas, are benign tumors of vascular origin that arise from neural crest cells located on the promontory [1]. They most commonly present with pulsatile tinnitus, though hearing loss, pain and cranial neuropathies could also present in more advanced stages [2,3]. The treatment of choice consists of complete surgical excision via a transcanal or a postauricular approach [3,4]. This was traditionally done under microscopic vision, nevertheless, with the introduction of endoscopes in ear surgery, a total endoscopic tumor excision has been attempted. The first total endoscopic middle ear neoplasm removal was reported by Marchioni, et al. [5] in 2013 and since then a few other reports have been published. We present here three cases of GTT treated via a total endoscopic transcanal approach. A review of the relevant literature is also performed.
Case Report
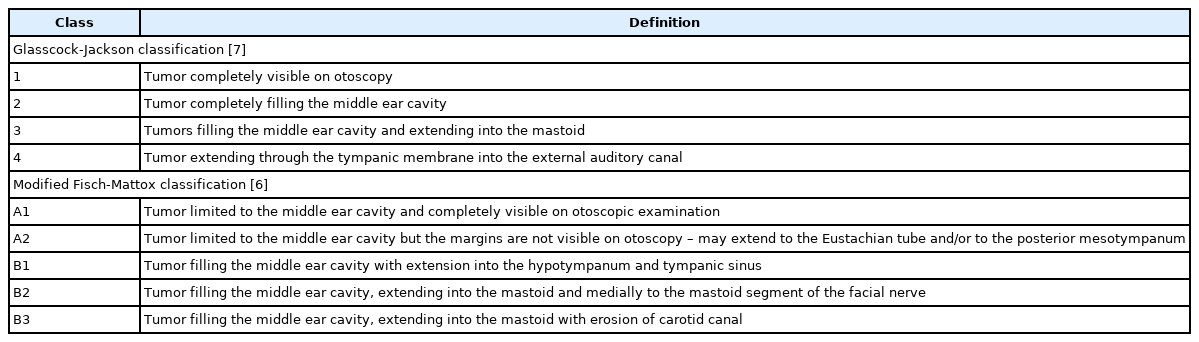
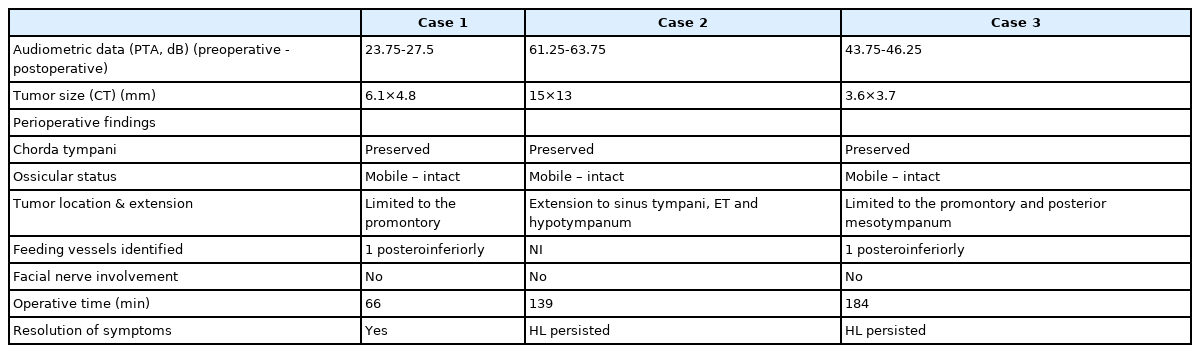
Case 1
A 74-year-old female patient was referred to our clinic with a clinical diagnosis of glomus tympanicum. She had a 3-year history of pulsatile tinnitus and fullness sensation in the left ear, as well as earache for the last 3 months. Otoscopy showed a reddish mass posterior to the tympanic membrane (Fig. 1A). Pure-tone audiometry revealed a left-sided mild sensorineural hearing loss in the 3-4 kHz frequency (Fig. 1B) while her tympanogram was A type. CT showed a mass measuring 6.1×4.8 mm adherent to the promontory (Fig. 1C). The mass was classified A1, according to the modified Fisch-Mattox (mFM) classification [6], and I, according to Glasscock-Johnson (GJ) classification [7] (Table 1). Surgical excision of the tumor was performed endoscopically and it was sent for pathological examination, which confirmed the diagnosis of GTT. No complications occurred and the patient showed no signs of recurrence after 2 years (Fig. 1D, Table 2).
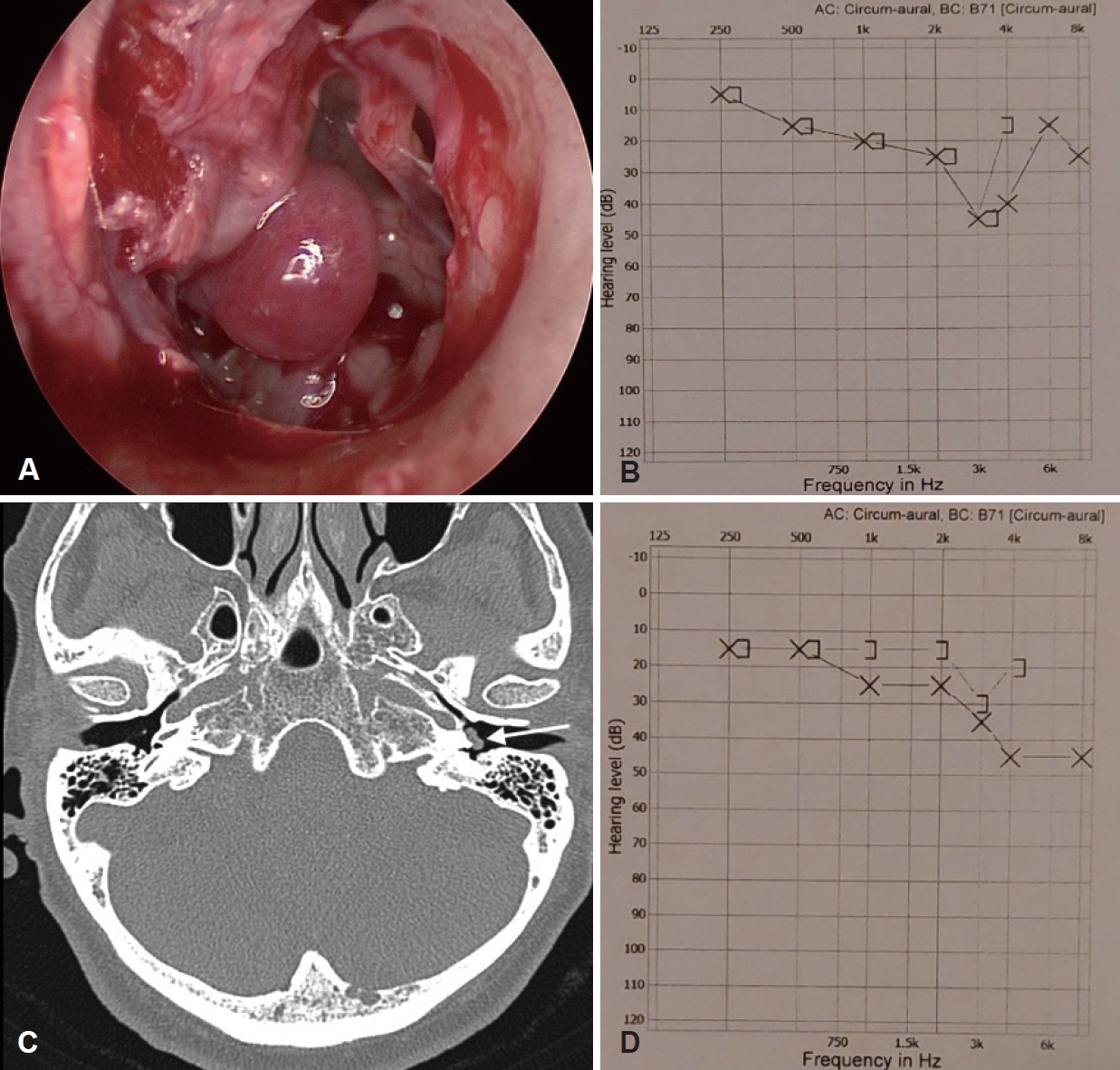
Case 1. A: Endoscopic image (Glasscock-Jackson classification I). B: Preoperative pure-tone audiogram. C: CT image showing the tumor (arrow) adherent to the promontory. D: Postoperative pure-tone audiogram.
Case 2
A 56-year-old female patient presented to the outpatient setting, complaining about pulsatile tinnitus, ear fullness, and a sensation of hearing loss. A red mass located in the middle ear appeared in otoscopy (Fig. 2A). Pure-tone audiometry revealed a left-sided moderately severe conductive hearing loss (CHL) in all frequencies (Fig. 2B) whereas her tympanogram was B type. Nonspecific findings of soft tissue density in the left middle ear and mastoid were shown in CT. MRI revealed a mass in the left middle ear, in touch with the promontory, enhancing post gadolinium (Fig. 2C). A clinical diagnosis of GTT (mFM class Β1, GJ class II) was made based on clinical examination and MRI, and the patient was planned for surgery. The mass was removed endoscopically and uneventfully, and the histopathological examination confirmed the diagnosis. The patient showed no signs of recurrence on a 14-month follow-up, although CHL persisted (Fig. 2D, Table 2). Otoscopy revealed a retraction pocket adherent to the promontory and the patient was offered a tympanoplasty, which she refused.
Case 3
A 45-year-old female patient was referred to our clinic with a 2-year history of pulsatile tinnitus and hearing loss. A red mass located in the middle ear, attached anteriorly to a thinned tympanic membrane, appeared in otoscopy (Fig. 3A). Pure-tone audiometry revealed a left-sided moderate CHL in all frequencies (Fig. 3B), whereas her tympanogram was B type. The diagnosis of GTT (mFM class A2, GJ class I) was made based on clinical examination and imaging (Fig. 3C), and the patient was offered surgical excision. The mass was removed endoscopically along with the part of the thinned tympanic membrane which was firmly attached to the tumor therefore a cartilage tympanoplasty was performed to fix the perforation. Histopathological examination confirmed the diagnosis. The patient showed no signs of recurrence on a 13-month follow-up, although air conduction thresholds remained stable (Fig. 3D, Table 2).
Surgical technique
All procedures were performed under general anesthesia. None of the patients underwent preoperative angiography and embolization. A 3 mm 0° endoscope was used throughout the whole procedure and a 3 mm 30° endoscope was used at the end to check for tumor residues. Traditional ear surgery instruments, as well as instruments from the Panetti endoscopic ear surgery (EES) set, were used. The patient was placed in the supine position with the head turned 45° to the right. A solution of 1:100.000 epinephrine was injected into the external ear canal skin and the tympanomeatal flap was raised and elevated from the annulus. The tympanic membrane was then detached from the malleus and the tumor was removed from the promontory with a suction Rosen knife. In the first and third patients, the tumors were removed en bloc, while in the second one via piecemeal resection, due to its larger size and proximity to the ossicles. Hemostasis was achieved by leaning the monopolar diathermy tip against a suction catheter (Frazier suction tube, 5 French, coated with a Nelaton catheter), which was pushed on the tumor and its feeding vessels in the first two cases. The power was set at 18 W. In the third case, an ophthalmic bipolar diathermy (25G Diathermy probe DSP, Alcon/Grieshaber, Schaffhausen, Switzerland) was used. The endoscope was cleared with warm natural saline, when the image became obscure due to blood clots, even though the use of adrenaline-soaked cotton balls prevented this from frequently happening. After removal of the tumor, myringoplasty was performed with the use of a tragal cartilage graft, due to small perforations in the tympanic membrane. No bone drilling was applied throughout the whole procedure.
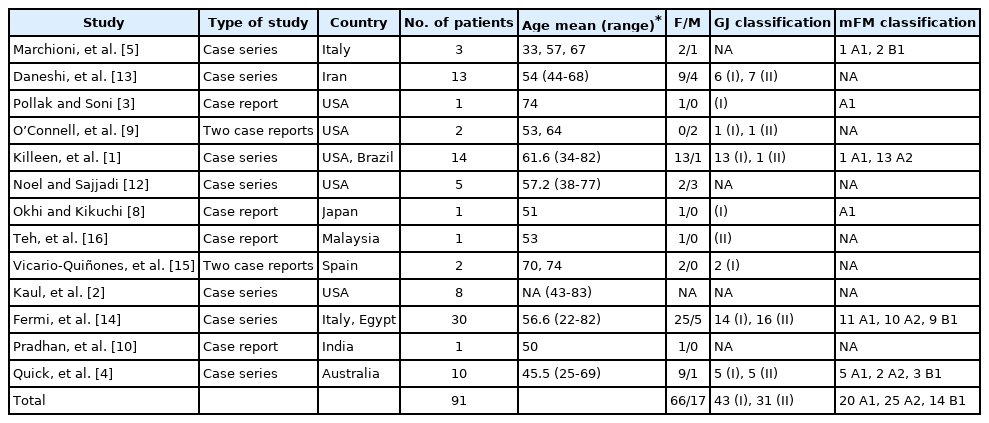
Discussion
EES has gained popularity over the last years, due to its advantages, which include a wide field of view, magnified vision, and the ability to visualize around corners [5,8,9]. As a result, its indications have expanded from cholesteatoma and stapes surgery to more complex procedures such as middle ear tumor excision and lateral skull base surgery, either via a total endoscopic approach or in combination with microscopic surgery [5,10,11]. GTT have as well been managed through an endoscopic approach and, since 2013, 13 studies have been published, to our knowledge, including 95 patients (Tables 3 and 4). An exclusive endoscopic excision was achieved in all patients, apart from one in the series of Noel and Sajjadi [12] and three in the series of Kileen, et al. [1]. The reasons, for which a postauricular microscopic conversion was needed, were tumor size in three cases and excessive hemorrhage in one case. One of the main challenges of GTT surgery is indeed its vascularity, which can result in significant bleeding. The most common methods, used for coagulation were bipolar cautery [4,5,13,14] and lasers. Argon plasma coagulation (APC) [13], diode [1], CO2 [1,3-5,15], and potassium titanyl phosphate (KTP) [1,2] lasers have all been used to achieve hemostasis. In two of our cases, a type of monopolar coagulation was used, by leaning the monopolar diathermy tip against a suction catheter. Generally, the use of monopolar cautery against the promontory is not advocated, as there is a risk of thermal injury in the fluids of the cochlea. In our two cases and in one case by Teh, et al. [16] that used the same method, hearing did not deteriorate postoperatively, nevertheless, monopolar cautery should be used with caution. For this reason, we set the power at a low value (18 W) and used it intermittently. To minimize this risk, in our third case, we used an ophthalmic bipolar diathermy. Of note, in one patient, in the series of Kileen, et al. [1], conversion to microscopic surgery via a transcanal approach was required to control bleeding. This problem was solved with the use of a “three-hand technique” in eight patients, in the series of Fermi, et al. [14]. It involves the use of a second surgeon that holds an extra instrument, to assist the primary surgeon. Total resection of the tumor was obtained in all studies presented, apart from three patients in the series of Fermi, et al. [14], because the tumors were closely related to the carotid artery. As for the complications, the most common one was tympanic membrane perforation in five patients [2,4,10,14,15], dysgeusia in four just from the series of Fermi, et al. [14], and hearing loss in one patient [5]. In our three cases, no major complications were recorded. Hearing thresholds remained stable or improved in the majority of patients, in the studies retrieved. A hearing deterioration of more than 10 dB was recorded in six patients and it was associated with tympanic membrane perforation in half of them. In our cases, two patients had CHL in all frequencies, preoperatively, which did not improve despite surgery. The reason in the second case was the medialization of the tympanic membrane, resulting in a retraction pocket adherent to the promontory. In the third case, no apparent reason was found, yet the patient declined surgical exploration. Operative time ranged from 45 to 248 minutes, but the higher values were affected by cases, in which conversion to microscopic surgery was undergone. EES has, on one hand, a positive effect on operative time, since postauricular approach and canalplasty can be spared. On the other hand, the use of just one instrument for dissection and hemostasis and the need of cleaning the endoscope tip from blood clots, prolong the procedure. Finally, tumor size is the main limitation of EES. The size of GTT in the studies retrieved from the literature review ranges from I to II in the GJ classification and from A1 to B1 in the mFM classification. Tumors extending into the mastoid or in the external auditory canal are more challenging to be managed in a total endoscopic approach. Careful preoperative evaluation and the ability to convert in microscopic surgery, when needed, are of utmost importance in such cases. EES is a safe and effective method of managing GTT. Its main limitation is tumor size, although tumors ranging from I to II in GJ classification and from A1 to B1 in mFM classification, can be completely removed endoscopically, in most cases. Hemostasis can be achieved with the use of lasers or electrocautery. Careful preoperative selection of patients, that could be managed endoscopically, ensures the best outcomes for the patients.
Acknowledgements
None
Notes
Ethics Statement
Written informed consent was obtained from the patients, for publication of these case reports and of the accompanying images.
Conflicts of interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Athanasios Luca Fountarlis, Charalampos Skoulakis. Data curation: Vasileios Lachanas, Ioannis Tsitiridis. Formal analysis: Athanasios Luca Fountarlis, Jiannis Hajiioannou. Methodology: Athanasios Saratziotis, Aggeliki Alagianni. Supervision: Aggeliki Alagianni, Jiannis Hajiioannou, Charalampos Skoulakis. Visualization: Athanasios Luca Fountarlis, Athanasios Saratziotis. Writing— original draft: Athanasios Luca Fountarlis. Writing—review & editing: Jiannis Hajiioannou. Approval of final manuscript: all authors.