|
 |
- Search
| J Audiol Otol > Volume 27(1); 2023 > Article |
|
Abstract
Background and Objectives
Hearing aid (HA) use is a common rehabilitation method for people with hearing loss. This study aimed to investigate whether the use of HA will advance the health-related quality of life (HRQoL).
Subjects and Methods
Patients referred to a public audiological department in Norway were invited to participate in this pre-post interventional study. The RAND-SF-36, a generic HRQoL questionnaire, was administered to the participants before and three months after HA fitting. Changes in HRQoL dimensions were analyzed for the whole group and for subgroups based on sex, age, and presence of tinnitus.
Results
A total of 202 adults (109 men; mean age, 66.68 years [SD=10.92]) were included in the study. After a mean observation time of 91.63 days (SD=45.61), pain and general health significantly improved. Women aged Ōēź70 years without tinnitus improved in social functioning, while men aged <70 years with tinnitus improved in general health.
Conclusions
Adults with mild hearing loss reported better general health and less bodily pain three months after HA fitting than before. The patient subgroups reported improved general health and social functioning. However, causation remains uncertain because of methodological limitations. A randomized, controlled trial with a longer follow-up time could clarify such issues.
Hearing loss is a large and increasing global health problem, leading to delayed language development, isolation, inferior academic performances and fewer employment options, among others [1]. As the prevalence increases with age, as much as two thirds of adults over 70 years of age probably have a clinically relevant hearing loss [2]. In the adult population, hearing loss is associated with problems such as social withdrawal and isolation, depression, cognitive decline, reduced quality of life, and familial stress [3-6]. Use of hearing aids (HAs) is a well-established rehabilitation method in adults with mild to moderate sensorineural hearing loss [7]. For conductive, asymmetric, and severe hearing losses, other interventions could be more appropriate.
Several reviews have studied the effect of HA use on healthrelated quality of life (HRQoL). Chisolm, et al. [8] found that HAs improve HRQoL by reducing psychological, social, and emotional effects of sensorineural hearing loss. In their systematic review, however, generic measurements did not improve after rehabilitation with HAs. In a Cochrane review including five randomized controlled trials, the authors concluded that HAs ŌĆ£are effective at improving hearing-specific healthrelated quality of life, general health-related quality of life and listening ability in adults with mild to moderate hearing lossŌĆØ [9]. The authors of this review found a small beneficial effect of HAs on HRQoL based on two studies. Listening ability was assessed using self-report outcome measures such as the Abbreviated Profile of Hearing Aid Benefit (APHAB). Nordvik, et al. [10] also did a systematic review, concluding that HA use seemed to improve general quality of life at follow-up within the first year.
The term HRQoL could be defined as the way health is empirically estimated to affect quality of life. It can be measured as general HRQoL, or disease specific HRQoL. In this study, we have used the well-known general HRQoL questionnaire RAND 36-Item Short Form Health Survey (RAND-SF-36) [11]. Of its eight dimensions (see Subjects and Methods), social functioning and general health perception assumingly would be most likely influenced by hearing loss, and maybe hearing rehabilitation. Clinically, patients with mild to moderate hearing loss often report social isolation and listening difficulties.
One might argue that the effect of HAs on HRQoL has been the subject of thorough investigation before, and is of little interest. However, as costs associated with hearing rehabilitation are substantial, and HA technology is improving, continuous attention to effects (or lack of effects) is warranted.
The aim of the present study is to explore whether general HRQoL improves in adults receiving HAs in our department, and if so, whether some groups of patients are more prone to improvement than others.
The survey was conducted in the audiology section of the otorhinolaryngology department at a public, secondary-level hospital in the north-western part of Norway. This is the only audiology department in this region, which means every person in need of hearing rehabilitation is referred here. The total population of the area is approximately 145,000, with a mix of urban and rural areas. The amount of new HA fittings per year is around 1,500 patients. HAs are publicly funded in Norway, but patients pay a fee for every appointment with the audiologist (corresponding to approximately $40).
Adults (Ōēź18 years old) granted with HAs on the basis of hearing loss were invited to join this pre-post interventional study. All patients had post-lingual hearing loss and were firsttime HA users. Aetiology of hearing loss was not considered for this study. Exclusion criteria were: no wish to participate, earlier HA use, dementia, or other conditions making them unable to answer the questionnaires.
When included, patients were asked to answer the RAND-SF-36 questionnaire on the day of HA fitting/adjustment. Fitting of HA was done as a non-structured agreement between the patient and audiologist based on individual hearing loss and patient preferences. After 2-4 months, patients had a follow-up appointment with their audiologist. This follow-up appointment serves mainly as a possibility to make minor HA adjustments and to resolve pertinent issues. Logging of HA use was not done, nor were any systematic tools used for HA verification and validation. They then answered another copy of RAND-SF-36. The questionnaire was in paper form and took patients around 10 minutes to complete. The patients could ask the audiologist if they had questions related to the form. Both the pre- and posttreatment appointments were done within the same environment and with the same audiologist. Additional information was retrieved from the patient records: age, sex, audiometric results, and symptoms. Data collection was performed between August 2018 and May 2020, but was not affected by the COVID-19 pandemic.
In terms of hearing loss, patients were grouped according to the World Health Organization classification, where mild hearing loss is pure tone average (PTA) up to 40 dB, moderate from 41 dB to 60 dB, and severe from 61 dB. The better ear was used for this grouping, and PTA was the average of hearing threshold levels at 500, 1,000, and 2,000 Hz. In addition to pure tone audiometry, speech audiometry was performed using the standard Norwegian three-word utterances list called ŌĆ£HiST speech audiometry.ŌĆØ These three-word utterances are intended for speech recognition threshold measurement. In addition to degree of hearing loss, patients were grouped in sensorineural, conductive, or mixed type of hearing loss.
RAND-36 is the non-commercial version of SF-36, hence we have used the name RAND-SF-36 throughout this article. It is a well-known and widely used generic HRQoL questionnaire [11]. It has been translated to Norwegian by The Norwegian Knowledge Centre for the Health Services (
https://fhi.no/en). The health survey consists of 36 items covering eight dimensions: physical functioning, role limitations due to physical problems, role limitations due to emotional problems, social functioning, emotional well-being, energy/fatigue (also called vitality), pain, and general health perceptions. The scoring was based on the RAND 36-Item Health Survey 1.0, details are found at the RAND Corporation webpage (https://www.rand.org/), as well as the English translation of the questionnaire. All scores were transformed into a 0 to 100 scale (worst to best), then the items belonging together were averaged into their respective dimensions.
Results from RAND-SF-36 at baseline and at follow-up were examined using paired-samples t-tests. Calculations were done for the whole study population, and after adjusting for sex, age, and tinnitus.
A 90% power with a two-sided level of significance of 5% was chosen. Stark and Hickson [7] reported a difference of -0.94 (SD 2.91) in the general health dimension pre- vs. postHA fitting. We therefore calculated with a mean of difference 1 (SD 3) and found a required sample size of 97 random pairs. Due to considerable uncertainty, we chose to include substantially more patients.
Statistical significance was defined as p<0.05. Statistical analyses were performed with SPSS 25.0 (IBM Corp., Armonk, NY, USA).
The study was approved by the Regional Committee for Medical Research Ethics (Ref. no 2018/933). Patients gave written consent after receiving oral and written information about the study. They were informed of all aspects of the study, including the aim of reviewing the effect of HAs on HRQoL.
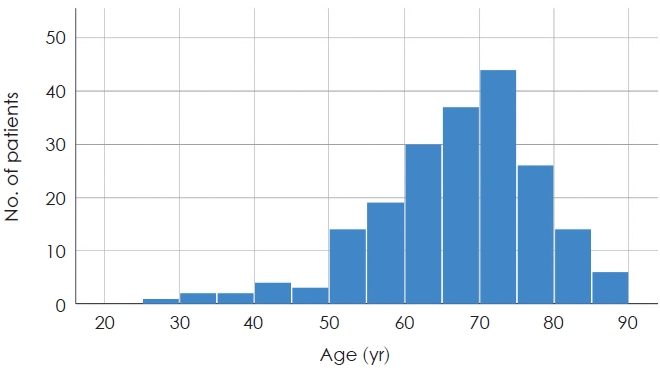
A total of 202 patients were included in the study; 109 (54.0%) were males. Mean age was 66.68 years (SD=10.92), Fig. 1 for age distribution. Mean follow-up time was 91.63 days (SD=45.61). Mean PTA for the study group was 25.90 dB (SD=10.98) (right) and 27.64 dB (SD=14.31) (left). PTA ranged from 0 dB to 53 dB in the better ear. All patients received HAs on both ears. Other descriptive details are presented in Table 1.
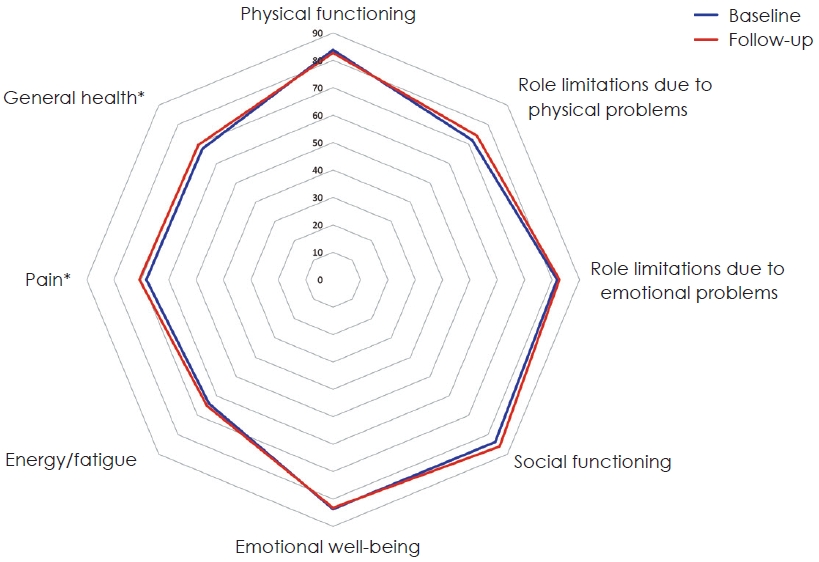
For the whole study population, two dimensions of RAND-SF-36 improved significantly at follow-up compared to baseline, namely pain, t(201)=-2.04, p=0.04, and general health, t(201)=-2.52, p=0.01. For the other dimensions, no significant changes were found (Fig. 2, Table 2).
Males reported significant improvement of general health, t(108)=-3.18, p<0.01, at follow-up compared to baseline. When adjusting for age, this improvement was only significant for males <70 years of age, t(56)=-5.18, p<0.001, and when dividing into 10-year age intervals, the age group 60-69 years showed significant improvement of general health, t(34)=-3.22, p<0.01. After further adjustment, only males (<70) with tinnitus (vs. no tinnitus) showed significant improvement of general health, t(29)=-7.17, p<0.01.
Females reported significant improvement of social functioning, t(92)=-2.64, p<0.01. When adjusting for age, this improvement was only significant for females Ōēź70 years of age, t(37)=-5.59, p=0.01, and when dividing into 10-year age intervals, the age group 70-79 years showed significant improvement of social functioning, t(27)=-2.87, p<0.01. After further adjustment, only females (Ōēź70) with no reported tinnitus showed significant improvement of social functioning, t(25)=-5.29, p=0.04.
No improvement in pain was found when adjusting for tinnitus in the whole study population.
Our patients reported a significant improvement of the HRQoL dimensions pain and general health at follow-up around 3 months after HA fitting. Although significant, the changes are quite small (Table 2) with only a 2-point improvement in general health on the 0-100 scale. As visualized in Fig. 2, this is a small change, hence clinical value is uncertain.
Several literature surveys report that HAs improve HRQoL in adults with mild to moderate hearing loss [8-10,12], our results are thus in line with this.
HRQoL measures can be generic or disease specific. Generic measures such as RAND-SF-36 are less sensitive to the effects of hearing interventions [13], but were chosen in this study as to explore the impact of HAs on general health perception. Using generic measures also eases comparison between conditions/ diseases. However, different generic HRQoL measures (questionnaires) are known to emphasize slightly different aspects of quality of life, and one may therefore calculate varying utility scores within the same person, depending on which HRQoL measure is used [14].
Our patients reported less bodily pain at follow-up compared to baseline. As this effect might not be immediately conceivable, one could suggest a decrease in total ŌĆ£illnessŌĆØ burden in patients with other medical conditions as a possible explanation. Moreover, as tinnitus is associated with more bodily pain [15], a direct effect of HAs relieving tinnitus symptoms could be possible. In contrast with the other HRQoL dimensions, less pain was not associated with a specific group of patients, for instance sex, age, or tinnitus. This further implies a random association.
Some prior studies have used SF-36 to measure the effect of HAs on HRQoL. Joore, et al. [16] reported a significant improvement of the social functioning dimension 25 weeks after HA fitting in a group of 80 hearing-impaired adults. For the 93 participants investigated by Stark and Hickson [7], only a significant worsening of general health was seen 3 months postfitting of HAs. No other significant changes were found. However, a positive change was seen for hearing-specific quality of life, measured with the Hearing Handicap Inventory for the Elderly. In both these studies, the majority of patients received monaural HAs. Crandell [17] found no significant changes in SF-36 scores in 20 elderly people with mild to moderate hearing loss after HA fitting, measured after 3 and 6 months. The hearing-specific APHAB, however, showed significant improvement. Together with our minor findings of improvement, as well as the knowledge of larger reviews showing improvement of other generic HRQoL measures after HA fitting, one might speculate that the RAND-SF-36 shows very little sensitivity to hearing-related aspects of HRQoL. However, as shown in an article using SF-36, hearing impairment is associated with poorer HRQoL than normal hearing [5]. According to these studies, HRQoL seems to be worser as the hearing impairment is greater.
After adjusting for sex, age, and tinnitus, we found two subgroups who improved significantly: younger than average men with tinnitus reported improved general health; and older than average women, without tinnitus, reported improved social functioning.
Tinnitus is known to affect men more than women, and is correlated with age, although a decline in severity is found in the oldest [18]. In a large cohort of older adults, Nondahl, et al. [15] found that increasing tinnitus severity was associated with lower HRQoL as measured with SF-36. HA is generally considered a good intervention in patients with hearing loss and tinnitus, although tinnitus treatment with HA showed questionable effect in a systematic review [19]. Whether it was an effect on tinnitus that caused the positive effect in our male tinnitus subgroup remains unanswered.
Males and females reported different effect of HAs in our study: younger than average men with tinnitus reported improved general health, while older than average women without tinnitus reported better social functioning. Niemensivu, et al. [20] found a positive effect of HA use on hearing-specific quality of life, but only women reported improvement in general HRQoL. However, in another Finnish study, the authors found improvement in HRQoL for men, but not for women [21]. A recent study comprising 105 adults (>60 years) assessed quality of life before and after HA fitting, using the World Health Organization Quality of Life-Adults module [22]. The domain ŌĆ£social participationŌĆØ was improved in women. This corresponds with our finding of improved social functioning in older women after HA fitting. Indeed, a cross-sectional analysis found that especially among older women, a strong association was seen between social participation and self-rated good health [23].
This study has several limitations. First, the study has no matched control group. This could have helped us discover random variations in HRQoL. Second, as there was no blinding, a response bias could have weakened our results because of the ŌĆ£honeymoonŌĆØ effect. However, blinding of HA use is practically difficult. Third, we did not control for actual HA use during the intervention time. It is a well-known fact that many people do not use their HAs. However, our clinical experience is that most new receivers use their HAs quite eagerly the first period of time.
An improved, future study would include a control group, add hearing-specific measures for quality of life, use HA verification, and have a longer follow-up time.
In conclusion, in this pre-post interventional study, younger than average males (<70 years) with tinnitus reported improvement in general health, while older than average females (Ōēź70 years) without tinnitus reported improvement in social functioning, three months after fitting of HAs. The results of this study should be interpreted with caution due to methodological limitations. A randomized, controlled trial with a longer follow-up time could clarify such issues.
Acknowledgments
The author is grateful to the departmentŌĆÖs audiologists for their practical help and support.
Fig.┬Ā2.
Radar chart comparing mean RAND 36-Item Short Form Health Survey (RAND-SF-36) dimensions at baseline (blue) and followup (orange). *Statistically significant changes.
Table┬Ā1.
Descriptive demographics of the patients included in the study
Table┬Ā2.
Paired-samples t-tests comparing means of RAND 36-Item Short Form Health Survey (RAND-SF-36) dimensions at baseline and on follow-up (n=202)
| Dimension | Baseline | Follow-up | p |
|---|---|---|---|
| Physical functioning | 83.76 (18.25) | 82.70 (19.88) | 0.08 |
| Role limitations due to physical problems | 71.91 (38.39) | 74.26 (37.40) | 0.32 |
| Role limitations due to emotional problems | 81.85 (33.26) | 82.67 (33.29) | 0.70 |
| Social functioning | 83.79 (20.30) | 86.05 (19.35) | 0.05 |
| Emotional well-being | 83.62 (13.08) | 83.18 (13.97) | 0.53 |
| Energy/fatigue | 64.01 (18.57) | 65.10 (18.08) | 0.26 |
| Pain | 68.16 (24.67) | 70.74 (24.05) | 0.04* |
| General health | 67.45 (16.47) | 69.48 (18.57) | 0.01* |
REFERENCES
1. Olusanya BO, Davis AC, Hoffman HJ. Hearing loss: rising prevalence and impact. Bull World Health Organ 2019;97:646



2. Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med 2011;171:1851ŌĆō2.



3. Kramer SE, Kapteyn TS, Kuik DJ, Deeg DJ. The association of hearing impairment and chronic diseases with psychosocial health status in older age. J Aging Health 2002;14:122ŌĆō37.



4. Uhlmann RF, Larson EB, Rees TS, Koepsell TD, Duckert LG. Relationship of hearing impairment to dementia and cognitive dysfunction in older adults. JAMA 1989;261:1916ŌĆō9.


5. Chia EM, Wang JJ, Rochtchina E, Cumming RR, Newall P, Mitchell P. Hearing impairment and health-related quality of life: the Blue Mountains Hearing Study. Ear Hear 2007;28:187ŌĆō95.


6. Scarinci N, Worrall L, Hickson L. Factors associated with third-party disability in spouses of older people with hearing impairment. Ear Hear 2012;33:698ŌĆō708.


7. Stark P, Hickson L. Outcomes of hearing aid fitting for older people with hearing impairment and their significant others. Int J Audiol 2004;43:390ŌĆō8.


8. Chisolm TH, Johnson CE, Danhauer JL, Portz LJ, Abrams HB, Lesner S, et al. A systematic review of health-related quality of life and hearing aids: final report of the American Academy of Audiology Task Force on the health-related quality of life benefits of amplification in adults. J Am Acad Audiol 2007;18:151ŌĆō83.


9. Ferguson MA, Kitterick PT, Chong LY, Edmondson-Jones M, Barker F, Hoare DJ. Hearing aids for mild to moderate hearing loss in adults. Cochrane Database Syst Rev 2017;9:CD012023


10. Nordvik ├ś, Laugen Heggdal PO, Br├żnnstr├Čm J, Vassbotn F, Aarstad AK, Aarstad HJ. Generic quality of life in persons with hearing loss: a systematic literature review. BMC Ear Nose Throat Disord 2018;18:1




11. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473ŌĆō83.

12. Johnson CE, Danhauer JL, Ellis BB, Jilla AM. Hearing aid benefit in patients with mild sensorineural hearing loss: a systematic review. J Am Acad Audiol 2016;27:293ŌĆō310.


13. Bess FH. The role of generic health-related quality of life measures in establishing audiological rehabilitation outcomes. Ear Hear 2000;21(4 Suppl):74SŌĆō9S.


14. Barton GR, Bankart J, Davis AC. A comparison of the quality of life of hearing-impaired people as estimated by three different utility measures. Int J Audiol 2005;44:157ŌĆō63.

15. Nondahl DM, Cruickshanks KJ, Dalton DS, Klein BE, Klein R, Schubert CR, et al. The impact of tinnitus on quality of life in older adults. J Am Acad Audiol 2007;18:257ŌĆō66.


16. Joore MA, Brunenberg DE, Chenault MN, Anteunis LJ. Societal effects of hearing aid fitting among the moderately hearing impaired. Int J Audiol 2003;42:152ŌĆō60.

17. Crandell CC. Hearing aids: their effects on functional health status. Hear J 1998;51:22ŌĆō4.
18. Bhatt JM, Lin HW, Bhattacharyya N. Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol Head Neck Surg 2016;142:959ŌĆō65.



19. Sereda M, Xia J, El Refaie A, Hall DA, Hoare DJ. Sound therapy (using amplification devices and/or sound generators) for tinnitus. Cochrane Database Syst Rev 2018;12:CD013094


20. Niemensivu R, Manchaiah V, Roine RP, Kentala E, Sintonen H. Health-related quality of life in adults with hearing impairment before and after hearing-aid rehabilitation in Finland. Int J Audiol 2015;54:967ŌĆō75.


21. Vuorialho A, Karinen P, Sorri M. Effect of hearing aids on hearing disability and quality of life in the elderly. Int J Audiol 2006;45:400ŌĆō5.