Cochlear Implantation in the Elderly: Speech Performance, Associated Factor, Complication, and Surgical Safety
Article information
Abstract
Background and Objectives
The guidelines for cochlear implantation (CIs) are expanding, and the number of CI procedures performed on the elderly is increasing. The purpose of this study was to analyze the results and safety of cochlear implantation in the elderly, as well as to evaluate the predictive factors on CI outcomes.
Subjects and Methods
The study included 56 patients aged ≥40 years, who received CIs between 2009 and 2020. They were divided into two groups: 27 younger adults (40-64 years) and 29 elderly (>64 years). The study compared their pre- and postoperative speech perception and category of auditory performance (CAP) scores, surgical complications, and hospitalization periods. It also evaluated associated factors in the elderly group by examining categorical and continuous variables and postoperative CAP score.
Results
There was a significant improvement in speech recognition tests (both word and sentence) and CAP scores in both groups compared to the pre-implantation scores (p<0.001). Postoperative results were slightly lower in the elderly group than in younger adults for sentence recognition and CAP scores, except for word recognition. No significant associated factors were found on postoperative CAP scores, except for etiology. Postoperative CAP significantly improved in the sudden hearing loss group compared to the groups with other etiologies (p=0.045). The elderly group had more comorbidities than that in the younger adult group (p=0.026), but there were no significant differences in postoperative complications and hospitalization periods.
Conclusions
While speech recognition and CAP scores were relatively lower in the elderly group compared to the younger adults, the elderly group showed significant improvements in audiological results after CI. Moreover, CI was safe and well tolerated in elderly patients.
Introduction
The prevalence of hearing impairment is increasing as the world population ages. According to the World Health Organization (WHO), one in four people will have some degree of disabling hearing loss by 2050 [1]. Globally, the prevalence of moderate-to-severe hearing loss increases exponentially with age, rising from 15.4% among people in their 60s to 58.2% among those aged over 90 years [1].
Hearing impairment has become a crucial topic for consideration in the geriatric population. The impact of acquired hearing loss in older adults is far-reaching, leading to communication difficulties, social isolation, economic burden, lower quality of life, cognitive impairment, and even dementia [2-5]. Hearing rehabilitation can provide a therapeutic approach for mitigating these risks [4,6-8]. Conventional hearing aids may be used in cases of mild-to-moderate sensorineural hearing loss (SNHL) [6]. However, in cases where hearing loss is more severe to profound, conventional hearing aids often become a nuisance without significantly improving speech discrimination or communicative skills [9,10]. Among many older adults with severe-to-profound SNHL, cochlear implantation (CI) may provide a more effective intervention than conventional hearing aids [8]. Recently, the guidelines for CI are expanding, and the number of CI procedures performed on the elderly is increasing [11,12]. Multiple studies provide evidence that CI among the elderly is relatively safe and can restore adequate social hearing function, with overall audiological outcomes comparable to those obtained for younger adults [11-13]. On the other hand, some studies that performed demographic comparisons of CI performance showed significantly worse postoperative performance in older adults [5,14-16]. Therefore, careful consideration should be given to the balance between the potential impact of any associated comorbidities and the long-term benefit of CI in elderly individuals, as well as the potential risks of surgery. Thus, the efficacy of CI in the elderly continues to be debated in the CI literature.
The major objectives of this retrospective study are to compare the audiologic results and safety of younger adults and elderly patients who received CI at our center, and to confirm the performance of CI in elderly patients. In addition, this study aims to explore the impact of predictive factors on CI outcomes of elderly patients because there is limited information in the literature on whether and to what extent preoperative features may influence the functional audiological efficacy of a cochlear implant.
Subjects and Methods
Patients and study design
A retrospective study was conducted on all CI recipients who were 40 years of age or older at the time of their surgery and were implanted at a tertiary hospital between January 1, 2009 and December 31, 2020. Data were collected from January 1, 2010 to December 31, 2021 to allow for a minimum follow-up period of 1 year. The data were extracted from the audiometry database and electronic patient management system. Approval was obtained from the Institutional Review Board of Kyungpook National University Hospital (IRB 2022-07-013). Since this is a retrospective analysis using data acquired during the treatment process of patients who have already undergone surgery, informed consent was not obtained. A total of 56 patients were included in this study and divided into two groups: younger adults (40–64 years; n=27) and the elderly (>64 years; n=29). All patients included in the study had postlingual deafness and were unilaterally implanted. Excluded patients consisted of those with prelingual deafness, patients with bilateral implants, those with mental retardation or handicap, and those with a lack of pre-implantation or adequate follow-up data. The patients underwent CI due to permanent severe-to-profound SNHL in both ears and did not benefit significantly from using conventional hearing aids for more than 3 months.
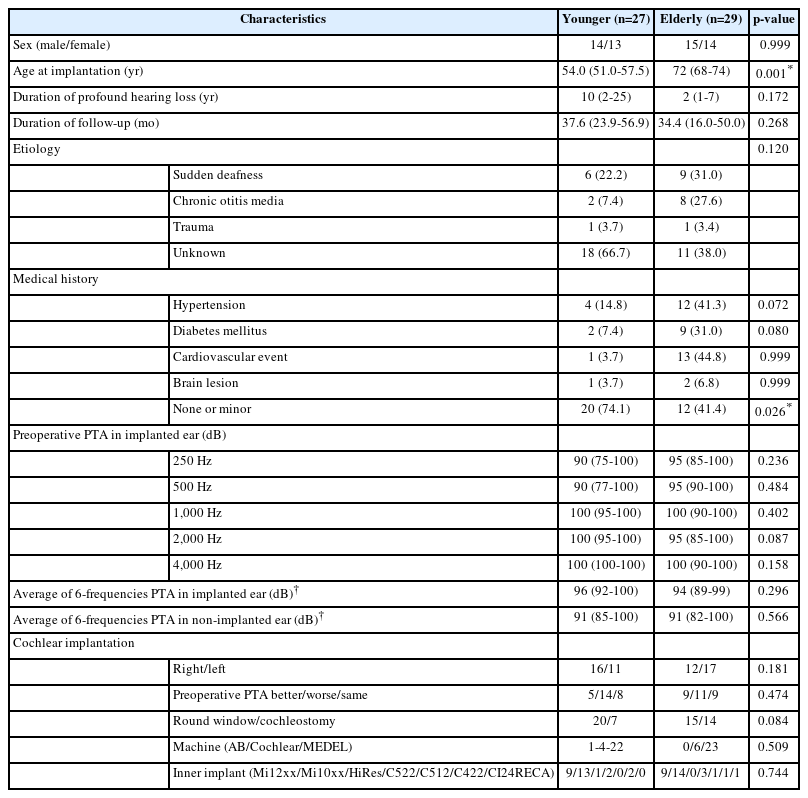
Demographic and clinical information was collected for each patient, including sex, age at the time of implantation, side of implantation, duration of profound hearing loss in the implanted ear, etiology (sudden deafness, chronic otitis media, trauma, unknown), medical history (hypertension, diabetes mellitus, cardiovascular events), preoperative pure tone average (PTA) in both ears, and characteristics of the implant.
The functional audiological outcome of CI was evaluated using postoperative speech perception scores and the Category of Auditory Performance (CAP) value, with the highest score recorded during a follow-up period of more than 1 year after surgery. CAP is a nonlinear hierarchical measure of auditory performance that consists of eight categories ordered from 0 to 7 in increasing difficulty [17]. Speech recognition testing was conducted in a quiet space using the Korean version of the Evaluation of Auditory Response to Speech (EARSK), which includes 20 monosyllabic words and 30 open-set sentences [18]. We compared the above audiologic results of younger adults and the elderly.
Data analysis
The data were analyzed using IBM SPSS software (version 27.0; IBM Corp., Armonk, NY, USA). Categorical variables were expressed as counts (percentages) and Pearson’s χ2 or Fisher’s exact test was used to analyze categorical variables. The distribution of continuous variables was evaluated using the Kolmogorov-Smirnov test and all continuous variables had non-normal distribution. Continuous variables were expressed as median (interquartile range) and compared using Mann-Whitney U-test or Kruskall-Wallis test. For continuous variables, the Wilcoxon signed-rank test was used to compare continuous variables before and after surgery. Pearson’s correlation was used to assess the correlation between continuous variables. The level of statistical significance was set at p<0.05.
Result
Patients
A total of 56 patients aged 40 years and older were implanted at our institute between 2009 and 2020. This population was subdivided into two groups: younger adults aged 40–64 years (n=27) and elderly group aged >64 years (n=29). Table 1 summarizes the demographic data for each group. The median age of the younger adult group was 54 years and 72 years of the elderly group with a range between 65 and 83 years. There were no significant differences in duration of profound hearing loss, sex, etiology, preoperative PTA in either ear, or the characteristics of the implant between the two groups, except for medical history. Among the younger adult group, 20 patients (74%) had either no medical history or only minor medical issues, while in the elderly group, 12 patients (41.4%) had no meaningful medical histories. Therefore, the elderly group had a higher prevalence of significant medical histories compared to the younger adult group (p=0.026). In addition, the duration of the patient’s hearing aid use was excluded from the analysis because the number of patients for whom the exact duration was recorded was very few and the majority of cases were ambiguous.
Audiological outcome
Fig. 1 shows the distribution of postoperative CAP scores by age. The tendency in the total patient group demonstrates good performance, with a CAP score of 5 or higher achieved by most patients regardless of age. A CAP score of 5 indicates the ability to understand common phrases without lip-reading. But there was no significant association with the postoperative CAP scores by age.

The distribution of postoperative Category of Auditory Performance (CAP) score by age. Total patients (n=57): correlation coefficient=-0.191, p=0.158 (●: younger adults group, ▲: elderly group). CI, cochlear implantation.
Fig. 2 demonstrates the outcomes of speech recognition tests for monosyllabic words and sentences, as well as CAP scores for both younger and elderly groups. As shown in Fig. 2, all postoperative functional audiologic tests in each group demonstrated statistically significant improvements compared to preoperative results. Both groups showed significant improvement (p<0.001) in the monosyllabic test (young: 12% [24%] vs. 72% [29%]; elderly: 8% [23%] vs. 67% [37%]). There was also significant improvement in sentence recognition after implantation in both groups compared to the preimplantation scores (p<0.001) (young: 0% [12%] vs. 90% [21%]; elderly: 0% [7%] vs. 79% [35%]). Additionally, postimplantation CAP scores showed a significant improvement (p<0.001) (young: 4 [0] vs. 7 [1]; elderly: 4 [2] vs. 6 [2]).
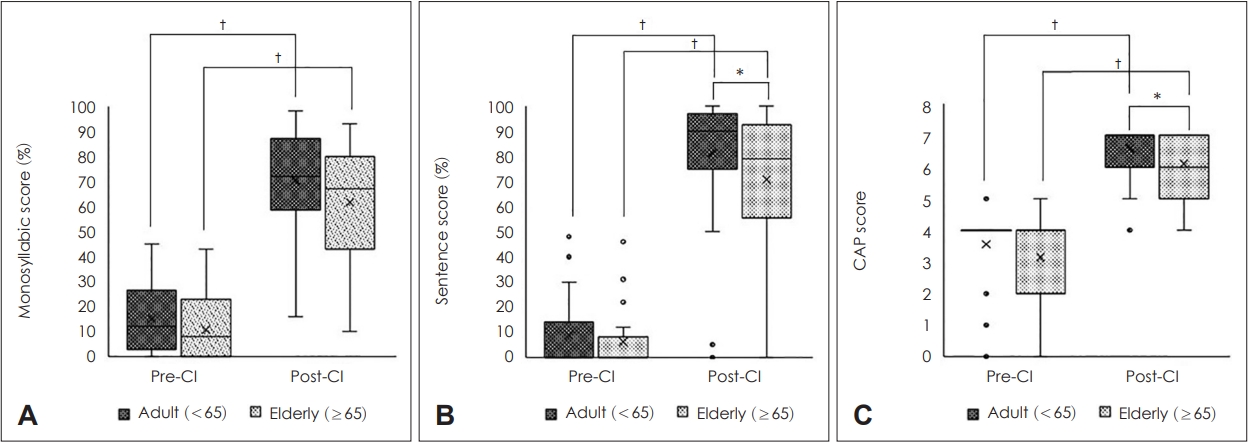
The improvement in younger and elderly patients for word (A), sentences (B), Category of Auditory Performance (CAP) score (C) after CI (*p<0.05; †p<0.001, statistically significant) (lower and upper sides of the box are the first [Q1] and third [Q3] quartiles). The box covers the interquartile range [IQR], where 50% of the data is found. The line that split the box in two is the median and “x” in the box means average. Mark data which fall below the lower bound and above the upper bound as outliers “o” [lower bound=Q1–1.5IQR, upper bound=Q3+1.5IQR]). CI, cochlear implantation.
There were no differences between the two groups in preimplantation scores for either word or sentence recognition, or CAP scores. However, the difference in postoperative outcomes between the two groups was statistically significant for sentence recognition and CAP scores, not word recognition scores (post-implantation word recognition: young vs. elderly=72% [29%] vs. 67% [37%], p=0.241; post-implantation sentence recognition: young vs. elderly=90% [21%] vs. 79% [35%], p=0.039; post-implantation CAP score: young vs. elderly= 7 [1] vs. 6 [2], p=0.029).
Postoperative complications and surgery safety
According to Chen’s classification, complications were categorized as minor or major based on their severity [16]. We investigated the incidence of complications according to this classification, and the results are shown in Table 2. In total, there were 2 major complications in 2 patients and 20 minor complications in 16 patients. The 2 major complications were electrode exposure and facial weakness, both of which occurred in the elderly group. The majority of the minor complications were postoperative vestibular symptoms, such as mild dizziness and troublesome tinnitus. Regarding vestibular symptoms, most patients experienced relief within 1 month after discharge, except for 1 patient who took several months to recover. Tinnitus cases were included when patients did not experience tinnitus before surgery but developed it after surgery, or when pre-existing tinnitus worsened after surgery.
Vestibular symptoms affected 14% (n=4) of the younger adult group and 20.6% (n=6) of the elderly group. Troublesome tinnitus affected 17.8% (n=5) of the younger adult group and 13.8% (n=4) of the elderly group. However, there was no statistically significant difference in the incidence of complications between the two groups.
We also investigated the hospitalization period of all patients to compare not only the side effects directly related to CI but also the complications attributable to general anesthesia and recovery time after surgery. The average hospitalization period for each group was 5.1 days (SD=1.66) for younger adults and 7.04 days (SD=4.28) for the elderly group. There was no statistically significant difference in hospitalization duration between the two groups.
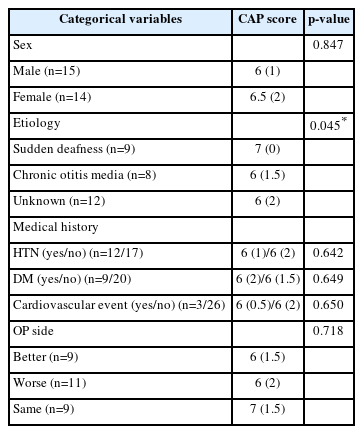
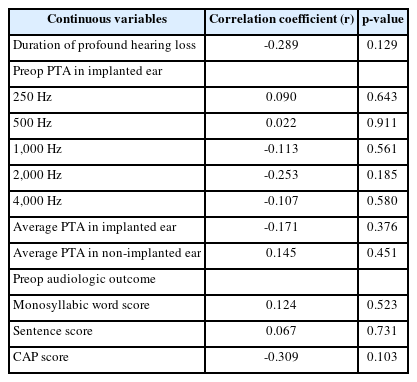
Associated factor of cochlear implant outcome
Lastly, we investigated the correlation between postoperative CAP and impact factors using four categorical variables and five continuous variables. Originally, we wanted to confirm the impact factor through multivariable analysis, but the number of patients who met the inclusion criteria was smaller than expected, so univariable analysis was performed to confirm the associated factor. The results of the four categorical variables of associated factors are shown in Table 3, and the five continuous variables of associated factors are presented in Table 4. In Table 3, sex, medical history (hypertension, diabetes mellitus, cardiovascular event), and implanted ear (worse, better, similar hearing) had no significant effect on postoperative CAP (p>0.05). However, postoperative CAP in the sudden hearing loss group showed a significant improvement compared to the other etiology groups (p=0.045). In Table 4, the duration of profound hearing loss showed a negative correlation with postoperative CAP, but it was not statistically significant. Additionally, none of the other continuous variables were statistically significant.
Discussion
The purpose of this study was to determine the influence of age on the functional audiological outcomes of patients after CI, as well as to identify predictive factors that influence postimplantation audiologic results. Additionally, the study aimed to assess the perioperative and postoperative complication rate in elderly patients and confirm the safety of surgery by analyzing operative complications.
In this study, both younger adult and elderly patients demonstrated good speech performance after surgery (Fig. 2). While elderly patients exhibited slightly poor results in sentence recognition, and CAP scores when compared to younger adult, their audiologic results was similar to that of elderly patients in a previous study. In the previous study, postoperative sentence recognition was 74.9% in younger adults (<70 years old) and 68.9% in older adults (≥70 years old) [14]. This suggests that CI yielded excellent results in both younger adult and elderly patients in this study, with only slightly lower results observed in elderly patients. And also, the difference in sentence recognition and CAP scores can be attributed to age-related differences in cognitive ability. Previous studies have shown that older adults exhibit lower speech performance compared to younger adults, indicating declines in speech perception and production abilities such as difficulty understanding speech, reduced ability to discriminate between similar sounds, slower speech rate, and less precise articulation [19,20]. These changes may be due to age-related changes in the auditory system, as well as cognitive processes involved in speech processing [21].
Many people tend to believe that older patients are at a higher risk of peri- and postoperative complications due to their comorbidities [16,22]. This study found no significant difference in peri- and postoperative complications between the elderly and younger adults. Recovery and anesthesia-related complication also showed no significant difference. Although there was no statistically significant difference in the risk of complication or hospitalization period between the two groups, two patients in the elderly group required a long hospitalization of more than 10 days. One patient had mild fever due to postoperative acute pyelonephritis and no additional problems after using antibiotics. The other patient developed non-ST segment elevation myocardial infarction after surgery and was transferred to the cardiology department for coronary angiography. Both patients had no history of cerebrovascular accident, did not take anticoagulants, and their renal function was within normal range. In particular, for elderly patients, regardless of the underlying disease, we thoroughly conduct postoperative laboratory tests and vital sign checks from the day of operation to discharge. Thanks to that, we were able to take quick action, and we were able to resolve the problem relatively without major complication.
Postoperative speech perception in elderly CI patients can be influenced by various internal and external factors, such as etiology, age at implantation, duration of hearing loss, degree of hearing loss, and residual hearing [23-25]. But our findings suggest that there is no statistically significant correlation between postoperative speech perception and age at implantation, duration of profound hearing loss, or preoperative audiologic results. These results are consistent with previous studies. Wong, et al. [13] divided a sample of elderly CI recipients into three age groups and reported no significant difference in audiological outcomes between the groups. Similarly, Favaretto, et al. [26] demonstrated that there were no significant associations between clinical features (age, sex, presence of comorbidities, and cochlear implant brand) and preoperative 6-frequency PTA.
We found that patients with sudden hearing loss had better postoperative hearing outcomes than those with other etiologies. There are few studies with the same conclusion as our study. Only one previous study, which divided patients into four groups according to etiology, showed that the speech recognition score of the progressive and sudden hearing loss group was superior to that of the prelingual hearing loss and meningitis groups [25]. In our study, sudden hearing loss group has shorter duration of profound hearing loss than the other etiology group (sudden HL group: 3.2±2.9 years vs. other etiology group: 11.1±17.2 years). Unlike etiology, there are many studies about relationship between duration of deafness and hearing outcomes after cochlear implant. Although our study could not confirm a statistically significant association, most studies found that patients with a shorter duration of deafness had better hearing outcomes after cochlear implant surgery than those with longer duration of deafness [23,27]. In conclusion, it is thought that the postoperative hearing results were good because the period of profound hearing loss was short in patients with sudden deafness, rather than the cause of sudden deafness itself having a good effect on the hearing results.
Limitations
This study has several limitations. The number of participants was lower than expected because only a few patients were able to provide all the necessary information for the study. Unfortunately, due to the relatively small number of patients involved, it was not possible to assess the individual impact of each factor using multivariate analysis. Furthermore, the retrospective study design may have affected the strength of the data. Therefore, our findings should be confirmed in larger cohorts using a prospective study design.
Conclusion
In this retrospective study, results showed significant improvement in audiological outcomes after CI in elderly patients, although speech recognition and CAP scores were slightly lower than in younger adults. In addition, CI was sufficiently safe and well tolerated in the elderly despite higher comorbidities.
Acknowledgements
This work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HR22C1832).
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Minji Oh, Kyu-Yup Lee. Data curation: Eun Jung Oh, Boseung Jung, Myung Hoon Yoo, Shin Young Yoo. Formal analysis: Minji Oh, Da Jung Jung, Kyu-Yup Lee. Funding acquisition: Kyu-Yup Lee. Methodology: Eun Jung Oh, Boseung Jung, Myung Hoon Yoo, Shin Young Yoo, Da Jung Jung, Kyu-Yup Lee. Project administration: Kyu-Yup Lee. Writing—original draft: Minji Oh, Kyu-Yup Lee. Writing—review & editing: Da Jung Jung, Kyu-Yup Lee. Approval of final manuscript: all authors.