Effects of Middle Ear Lesions on Pre and Postoperative Hearing Outcomes in Patients with Chronic Otitis Media
Article information
Abstract
Background and Objectives
The purpose of this study was to evaluate the effects of middle ear lesions on pre and postoperative hearing in patients with chronic otitis media (COM) and to assess the relationship between various prognostic factors and pre and postoperative hearing using more than 2000 COM surgery records retrieved from a computerized database released by the Korean Otologic Society in 2005.
Subjects and Methods
Data of 2312 COM surgeries, which had been conducted by a single surgeon from 1989 to 2009, were reviewed retrospectively. Mean preoperative and postoperative air-bone gap (ABG) was analyzed using a four-frequency (500, 1000, 2000, and 3000 Hz) pure tone average (PTA). Pre and postoperative ABGs were compared with regard to several prognostic factors, including disease duration, age, Eustachian tube function, existence of otorrhea, size of tympanic membrane perforation, degree of ossicular destruction, presence of cholesteatoma, and its type.
Results
Mean pre and postoperative ABGs of PTA in the 2079 cases studied were 27.88±13.33 dB and 17.38±15.64 dB, respectively, with a hearing success rate of 69%. The results suggested that preoperative ABGs were affected by Eustachian tube function, Griffin grade, presence of cholesteatoma and its type, and the degree of ossicular destruction. Hearing gains differed significantly among the groups when compared with factors of Griffin grade, presence or type of cholesteatoma, and the degree of ossicular destruction.
Conclusions
Many factors affected pre and postoperative ABGs and postoperative hearing outcomes. These results will be useful for designing future clinical studies on COM surgery, as well as for surgical planning and patient counseling in clinical practice.
Introduction
Chronic otitis media (COM) is an inflammatory disease of the middle ear with a prevalence rate of 2.57% according to a recent report by the Korean Ministry of Health and Welfare. COM is also a disease of conductive hearing loss and can be surgically treated. However, not all cases of hearing loss caused by COM can be corrected, and various prognostic factors can affect postoperative hearing outcome.
In general, middle ear lesions in patients with COM accompany structural changes that affect the sound transmission mechanism from the tympanic membrane to the oval window. These include destruction of the ossicular chain, tympanic membrane perforations, Eustachian tube dysfunction, and cholesteatomas.1) Mishiro, et al.2) reported that abnormalities of the ossicular chain are the most important factor affecting hearing outcomes after a long-term follow-up of >5 years. In contrast, Kim, et al.3) reported that the preoperative presence of cholesteatoma or otorrhea can affect postoperative hearing outcomes, and other reports also considered whether the status of middle ear mucosa, Eustachian tube function, and revision surgery can affect postoperative hearing.4) Although the types and severity of middle ear lesions are important factors affecting preoperative hearing status and postoperative hearing outcome, it is difficult to evaluate middle ear lesions accurately prior to surgery. LaRouere, et al.5) reported that high resolution three-dimensional computerized tomography (3D CT) scans of the temporal bone were useful for preoperative planning and pointed out that the findings estimated with 3D CT should be interpreted with caution because a discrepancy between image findings and actual lesions found during surgery is often observed. Large-scale clinical studies in Korea on COM prognostic factors are scarce, and the results of sporadic small-scale studies do not apply to actual clinical practice.
The aim of the study was to investigate the effect of middle ear lesions on pre and postoperative hearing using surgical records of >2000 cases of mastoidectomy with tympanoplasty conducted by one surgeon, which were retrieved from a computerized database released by the Korean Otologic Society in 2005.8)
Subjects and Methods
Subjects
This study was performed retrospectively using surgical records of 1907 patients (2079 ears) who underwent mastoidectomy with tympanoplasty and were followed up for 6 months or longer (range, 6-256 months; mean, 13.2 months) after surgery. All surgeries were conducted by one senior surgeon from 1989 to 2009. Surgical records consisting of patient demogra-phics, preoperative findings, intraoperative findings, and follow-up results were kept in storage and updated using a computerized database program released by the Korean Otologic Society in 2005.8)
Patients who had not undergone a mastoidectomy were excluded, and those who had experienced acute mastoiditis, traumatic tympanic membrane perforation, congenital middle ear cholesteatoma, or congenital ossicular anomaly were also excluded. Those who did not have postoperative follow-up data such as pure tone audiometric results and tympanic membrane findings at least 6 months after surgery were also excluded.
In total, 1907 patients (2079 ears) were included, and records were retrieved from the database pool of 2312 patients with COM. Among them, 913 were male (47.8%) and 1166 were female (52.2%). A total of 1021 (53.5%) patients had undergone left ear surgery, and 1058 (46.5%) had undergone right ear surgery. Surgery was performed once in 1907 (91.7%) ears, twice in 162 (7.8%) ears, and three times in 10 (0.5%) ears. Primary cases of cholesteatoma were present in 658 (31.6%) ears.
Diagnoses, histories, and physical examinations including otoscopy and pure tone audiometry were performed, and 3D CT scans of the temporal bone were conducted for surgical planning. All patients had diploic or sclerotic pneumatization with poor development of mastoid air cells.
Methods
Factor analysis
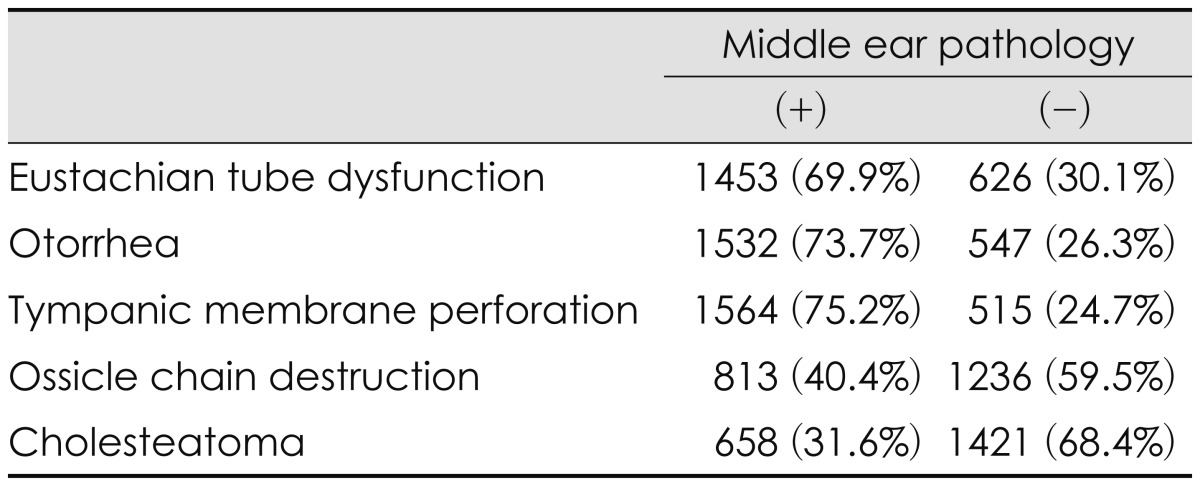
The parameters to be analyzed were divided into factors related to patients and those related to the middle ear lesions. The patient factors used were disease duration and patient age, and the middle ear lesion factors used were Eustachian tube function, the presence of otorrhea, size of the tympanic membrane perforation, types of ossicular injury, and the presence of cholesteatoma and its type (Table 1). Accordingly, patient hearing outcomes were compared between or among groups.
Disease duration was divided into the following categories: within 3 months, 3 months to 1 year, 1-3 years, 3-5 years, and >5 years after the first symptoms, and these categories included 208, 241, 185, 124, and 1321 cases, respectively. There were 57 cases of children aged <15 years and 2022 adults aged ≥15 years.
There were 626 cases of patent Eustachian tubes and 1453 cases in the obstruction group based on the nose Valsalva maneuver test. Preoperative otorrhea was found in 1532 cases (73.7%). The subjects who had otorrhea underwent a bacterial examination, followed by surgery after the surgical window was cleaned as much as possible using appropriate antibiotics and ear solutions. Tympanic membrane perforations were gra-ded using Griffin's classification system6): 313 (15%) cases of grade I (smaller than a 25% perforation of the tympanic membrane pars tensa), 642 cases (30%) of grade II (25-50% perforation), 337 cases (16%) of grade III (50-75% perforation), 272 cases (13%) of grade IV (75-100% perforation) or a marginal or pars flaccid perforation, and 515 cases (24%) of no perforation.
There were 291 cases (14%) of a destroyed incudo-stapedial joint with a lenticular process injury, 251 cases (12%) of a destroyed incus long process, 137 cases (6%) of a destroyed supra-structure of the stapes, 164 cases (7%) of the only footplate remaining, and 1236 cases (59%) of an intact ossicular chain. The mild group of ossicular destruction represented cases with only one ossicle injured, and the severe group represented cases with only the footplate remaining. Hearing comparisons were not conducted regarding the presence of the malleus handle.
The type of cholesteatoma was classified into attic cholesteatoma, sinus cholesteatoma, and tensa cholesteatoma. Attic cholesteatoma is characterized by the retraction or perforation of the pars flaccida. Sinus cholesteatoma is the retraction or perforation of the posterosuperior pars tensa of the tympanic membrane progressing from the sinus tympani and posterior tympanic cavity toward the mastoid. Tensa cholesteatoma is total retraction of the pars tensa of the tympanic membrane.7) The attic type, sinus type, and tensa type of cholesteatoma were observed in 383 (19%), 138 (6%), and 137 (6%) cases, respectively.
In total, 180 cases of exploratory tympanotomy with ossiculoplasty were performed in patients with non-inflammatory diseases, such as a congenital ossicular anomaly or traumatic ossicular disruption and were assigned to the control group. Hearing outcomes of 760 ossiculoplasty cases performed in patients with COM were compared with those of the control group to investigate the effect of inflammation on hearing outcome after surgery.
Hearing analysis
Pure tone audiometry was performed before and after surgery as a hearing assessment. The mean air conduction values and bone conduction thresholds at 500, 1000, 2000, and 3000 Hz were measured, and the mean pure tone average (PTA) and air-bone gap (ABG) were calculated: PTA=(500+1000+2000+3000)/4; ABG=mean postoperative air threshold-mean preoperative bone threshold. The success rates of postoperative hearing outcome were based on the guidelines for postoperative hearing reports (Korean Otological Society, 2005).8) If postoperative ABG was ≤20 dB, it was considered successful hearing. Postoperative ABGs were graded as ≤10 dB, 11-20 dB, 21-30 dB, or ≥31 dB, and each grade was considered the best outcome, good outcome, no change, or poor outcome, respectively.
Statistical analysis
The statistical analysis was performed using Windows SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA). The independent t-test and Scheffe's test with an analysis of variance were used to compare improvements in ABG. Spearman's correlation coefficient of cross-analysis was used to examine the postoperative hearing improvements. A linear regression analysis was used to exclude the influences of confounding variables. A p-value <0.05 was considered significant.
Results
Patient factors
Disease duration
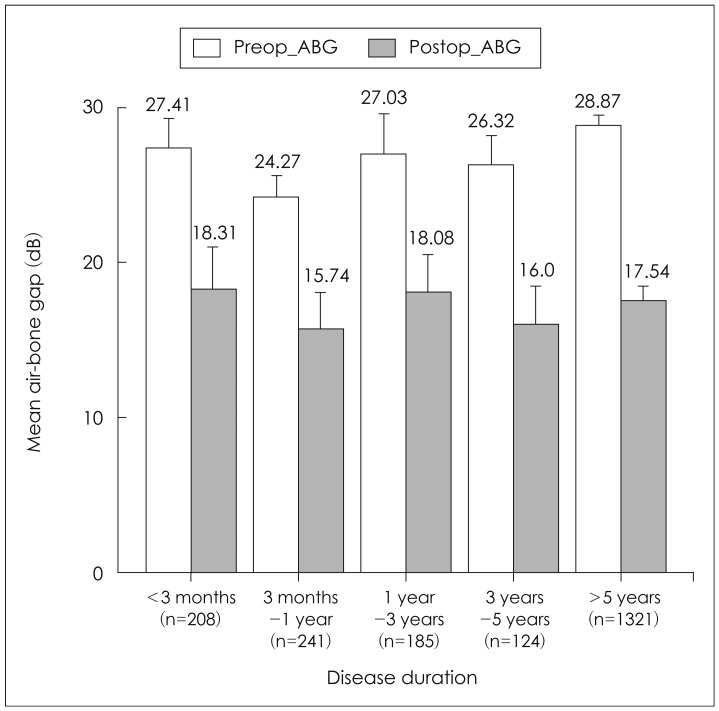
Pre and postoperative ABGs were 27.41±14.39 and 18.31±17.18 dB, respectively, with a disease duration <3 months, 24.27±11.14 and 15.74±16.19 dB with a disease duration of 3-12 months, 27.03±18.56 and 18.08±15.21 dB with a disease duration of 1-3 years, 26.32±10.89 and 16.0±13.10 dB with a disease duration of 3-5 years, and 28.87±13.33 and 17.54±15.62 dB with a disease duration of ≥5 years. No significant differences in postoperative hearing were found based on disease duration (p=0.431)(Fig. 1).
Age
Pre and postoperative ABGs were 28.18±15.66 and 20.70±15.02 dB, respectively, for patients aged <15 years (p=0.856), and 27.87±13.26 and 17.30±15.66 dB for those aged ≥15 years (p=0.175). No significant differences in pre and postoperative hearing were found (Fig. 2).
Middle ear lesion factors
Eustachian tube function
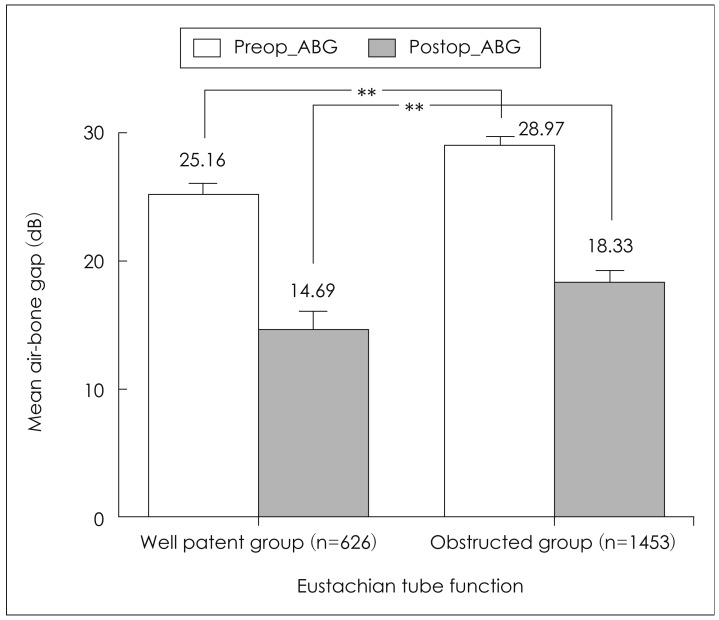
Pre and postoperative ABGs were 25.16±11.79 and 14.69±14.81 dB, respectively, in the patent group, and 28.97±13.85 and 18.33±15.86 dB in the obstructed group. Thus, the pre and postoperative ABGs were significantly lower in the patent group than those in the obstructed group (p<0.001), but no significant differences in hearing improvement were found between the two groups (Fig. 3).
Otorrhea
Preoperative ABGs were 27.51±11.93 dB in the otorrhea group and 28.92±16.50 dB in the nonotorrhea group, which was significantly different (p=0.028). But, no significant differences were found in the postoperative ABG between the groups (p=0.124)(Fig. 4).
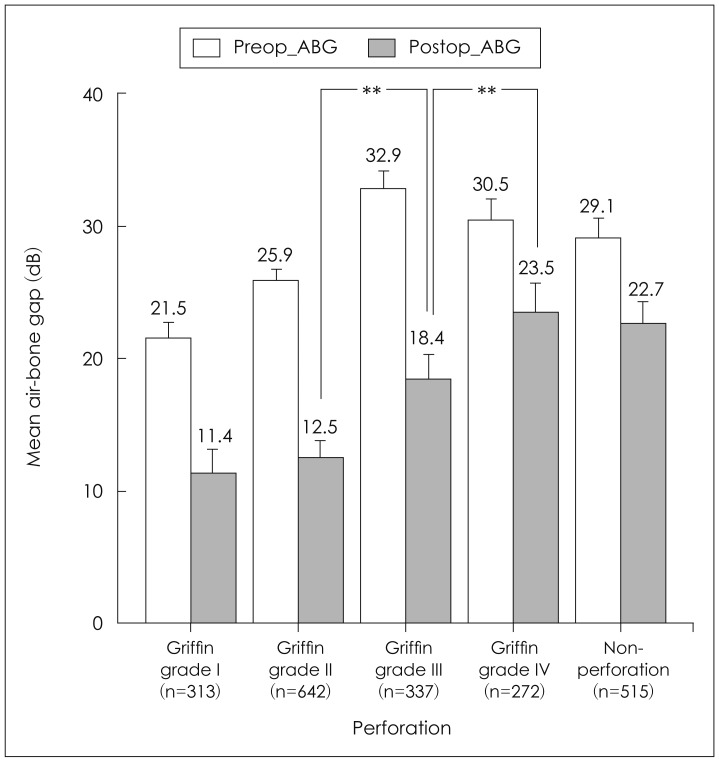
Severity of the tympanic membrane perforation
Pre and postoperative ABGs were 21.52±11.25 and 11.43±14.05 dB, respectively, in the Griffin grade I tympanic membrane perforation group, 25.90±10.50 and 12.52±13.93 dB in the grade II group, 32.86±12.36 and 18.44±15.46 dB in the grade III group, 30.46±13.80 and 23.49±16.10 dB in the grade IV group, and 29.08±19.50 and 22.66±15.58 dB in the control group without a perforation. No significant differences in the preoperative hearing were found between the groups, but better postoperative hearing outcomes were observed in patients with grade II compared with those who had grade III, as well as grade III compared with grade IV (Fig. 5).
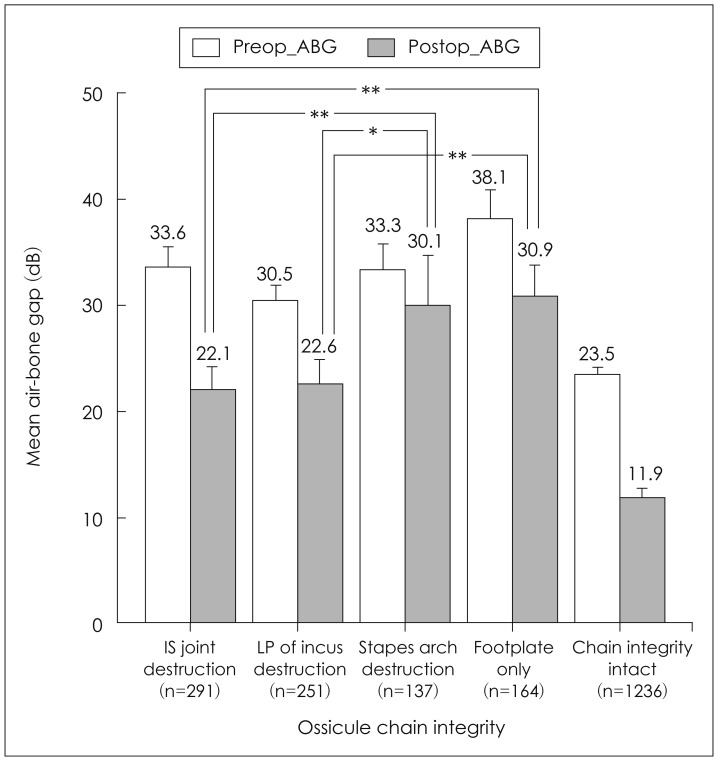
Ossicular injury type
Pre and postoperative ABGs were 33.63±15.94 and 22.12±15.04 dB, respectively, in the destroyed incudo-stapedial joint group, 30.47±10.91 and 22.61±14.95 dB in the destroyed incus long process group, 33.32±12.93 and 30.06±20.42 dB in the destroyed stapes supra-structure group, 38.15±16.60 and 30.89±14.38 dB in the footplate only left group, 33.52±14.52 and 24.95±16.19 dB in the entire ossicular injury group, and 23.46±11.38 and 11.39±13.30 dB in the no ossicular injury group. Pre and postoperative hearing levels were significantly different between the ossicular injury group and those without ossicular injury (p<0.05). When examined according to the ossicular injury type, no significant differences in preoperative hearing were found among the three mild ossicular destruction groups. However, ABG was significantly greater postoperati-vely in the destroyed stapes supra-structure group than that in the other groups (p<0.05)(Fig. 6).
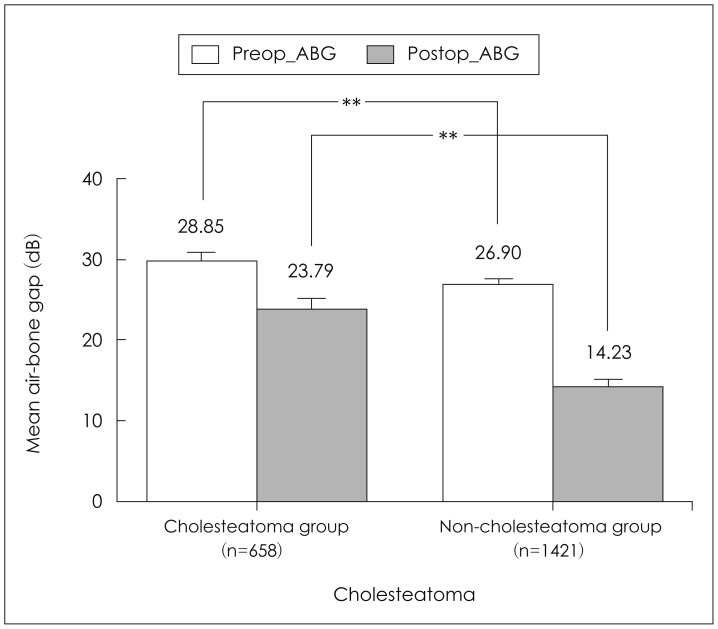
Presence of cholesteatoma
Pre and postoperative ABGs were 29.85±13.67 and 23.79±15.56 dB, respectively, in the cholesteatoma group and 26.90±13.10 and 14.23±14.74 dB in the non-cholesteatoma group. Pre and postoperative ABGs were significantly greater in the cholesteatoma group than those in the non-cholesteatoma group (p<0.001)(Fig. 7).
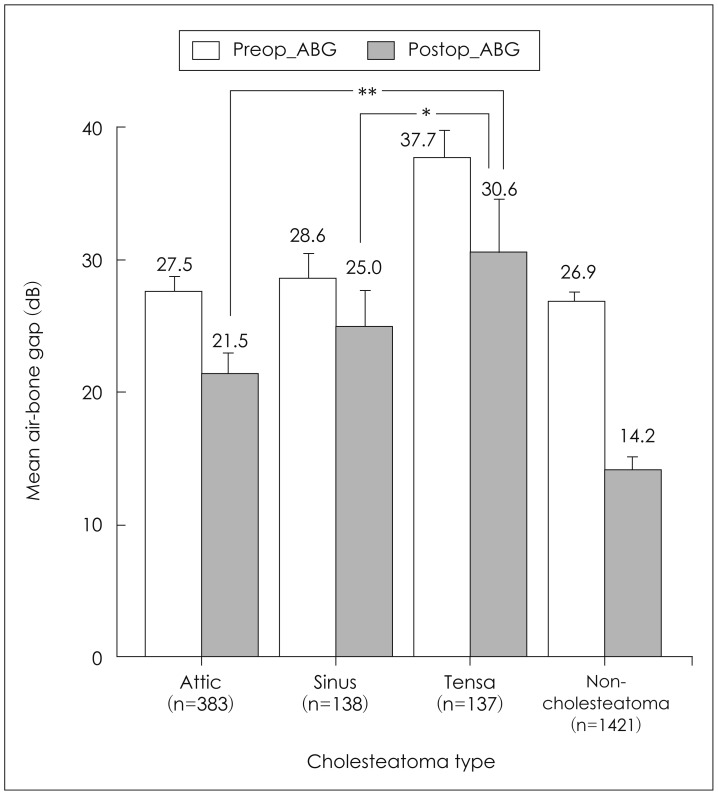
Type of cholesteatoma
Pre and postoperative ABGs were 27.47±13.70 and 21.45±14.19 dB, respectively, in the attic cholesteatoma group, 28.63±11.71 and 25.02±15.10 dB in the sinus cholesteatoma group, and 37.74±12.50 and 30.65±18.69 dB in the tensa cholesteatoma group. Patients in the tensa type cholesteatoma group showed a greater ABG post-operatively than those with other types of cholesteatoma (p<0.05)(Fig. 8).
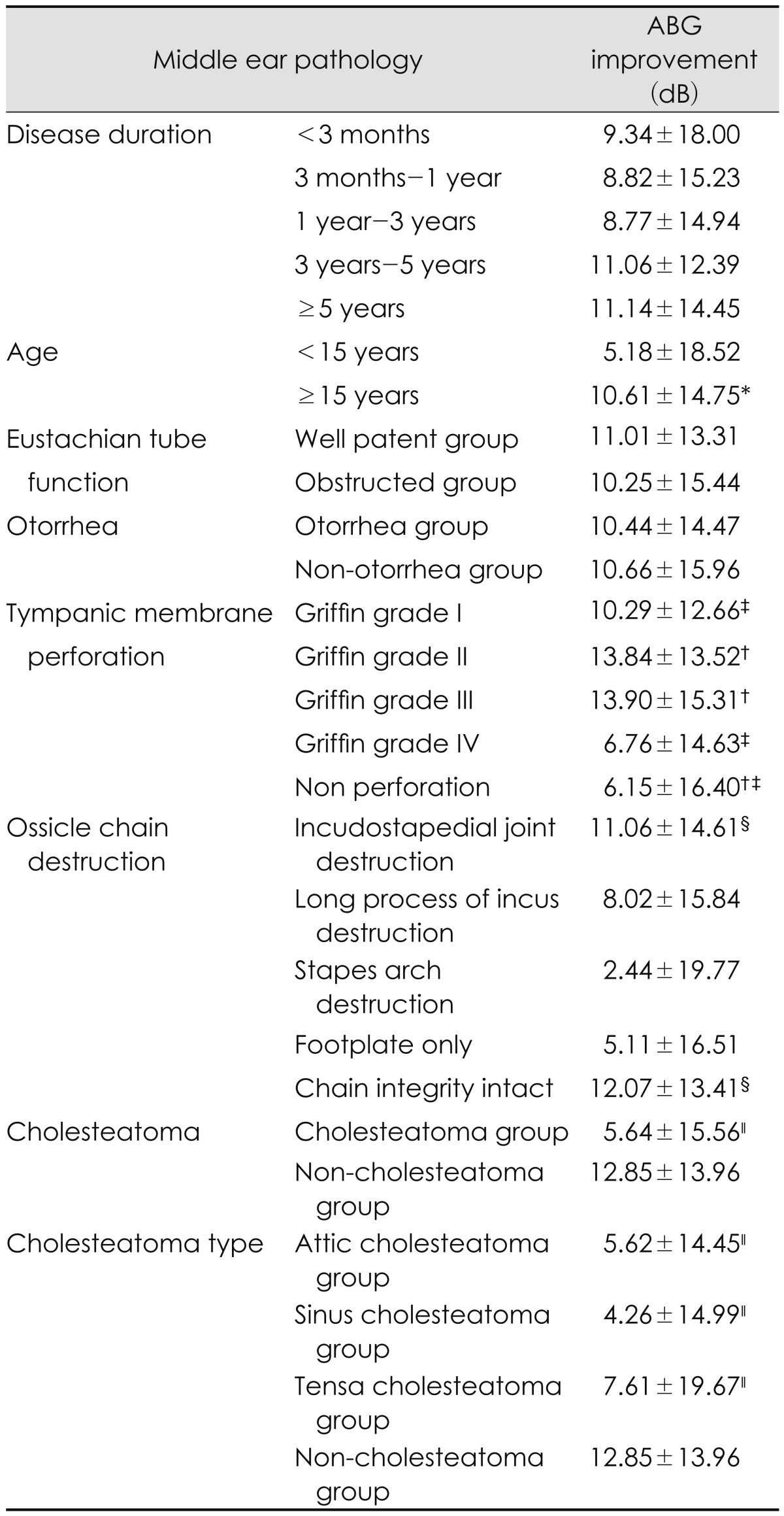
Inflammatory lesions
Pre and postoperative ABGs were 33.52±14.52 and 24.95±16.19 dB, respectively, in the ossiculoplasty in COM group, and 28.68±14.18 and 14.15±13.03 dB in the ossiculoplasty with no inflammatory disease group. The latter group showed significantly better hearing results compared to those in the former group (p<0.001)(Fig. 9). The ABG for each factor is presented in Table 2.
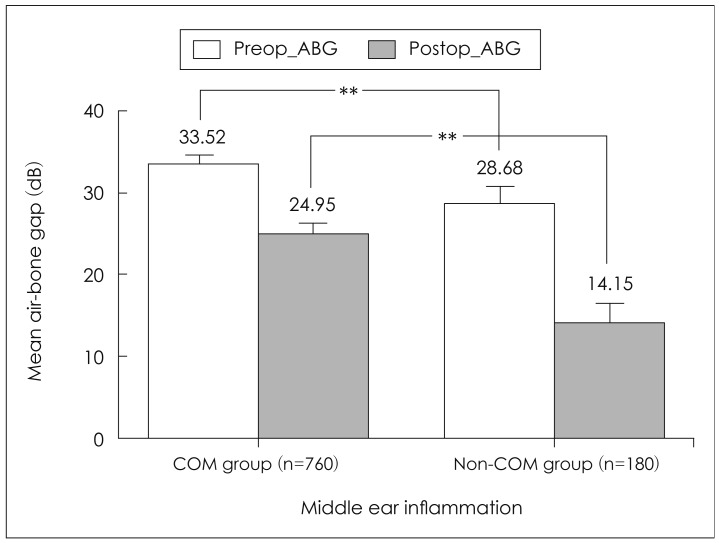
Mean pre and postoperative air-bone gaps (ABGs) according to the existence of middle ear inflammation. Postoperative ABGs in the chronic otitis media (COM) group were significantly greater than those in the group without COM (**p<0.001, independent t-test).
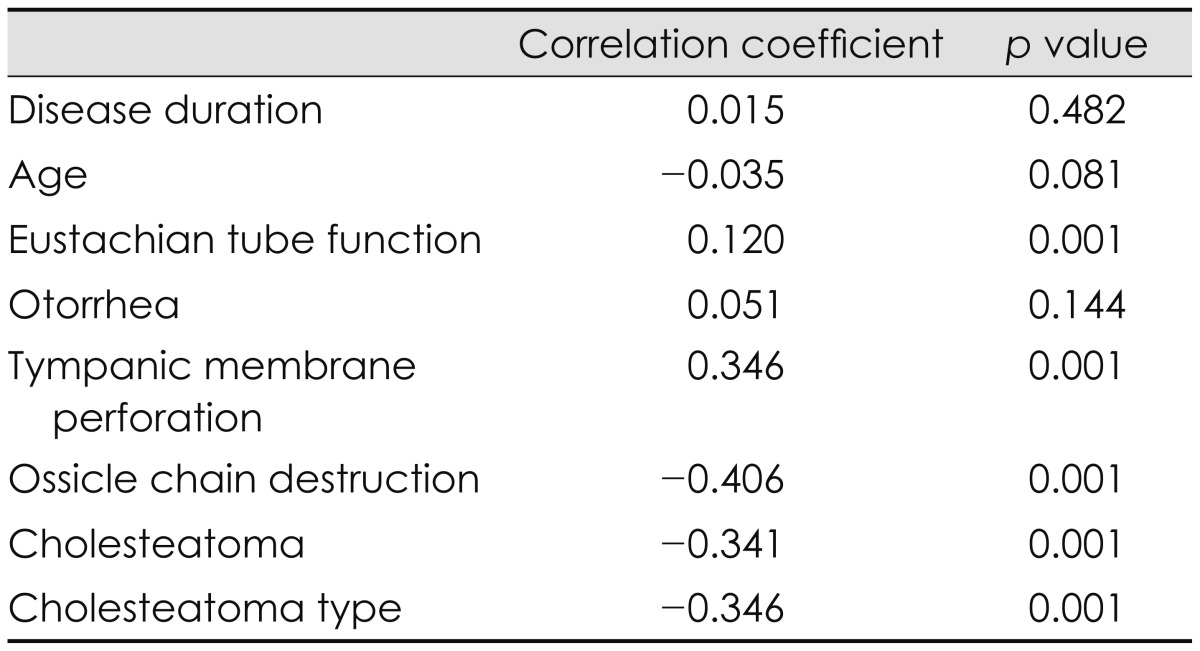
Factors related to pre and postoperative hearing
Post-operative hearing improvements were observed in 1435 (69.0%) of the 2079 cases. Mean pre and postoperative ABGs were 27.88±13.33 and 17.38±15.64 dB, respectively, in all patients, showing significant improvement after surgery (p<0.001). As successful hearing outcomes were analyzed using the ABG level,8) Eustachian tube function, Griffin grade of tympanic membrane perforation, presence of cholesteatoma, cholesteatoma type, and ossicular injury type were correlated with postoperative hearing improvement (p<0.001), unlike patients age (p=0.081), disease duration (p=0.482), and the presence of otorrhea (p=0.144)(Table 3).
Factors related to preoperative ABG in the linear regression analysis were Eustachian tube function, Griffin grade of the tympanic membrane perforation, presence of cholesteatoma and its type, and the presence of ossicular injury, whereas factors related to postoperative ABG were preoperative ABG, Gri-ffin grade of the tympanic membrane perforation, presence of cholesteatoma and its type, and ossicular injury type (p<0.05) (Table 4). The status of the postoperative hearing improvement for each factor is presented in Table 5.
Discussion
As COM may cause scar tissue formation in the middle ear mucosa, tympanic membrane perforation, and ossicular injury leading to conductive hearing loss, surgical interventions are required to eliminate the inflammation and improve hearing.9,10)
Hearing outcomes were poorer in the pediatric group than those in the adult group before and after surgery (Table 3). Previous studies have also reported that hearing improvements after COM surgery in pediatric patients were approximately half those of adult patients. Postoperative hearing outcome in young patients was probably due to disorders in Eustachian tube function caused by allergies. Eustachian tube dysfunction was also related to preoperative hearing level and postoperative hearing outcome in this study. Repetitive negative pressure occurs with Eustachian tube dysfunction, which may result in injury and fibrosis of the middle ear mucosa. Consequently, adhesion changes between the tympanic membrane and the ossicles may affect hearing.11) Some studies have reported a significant effect of Eustachian tube function on postoperative hearing, although other studies have reported that Eustachian tube function hardly affects postoperative hearing.12-14) These inconsistent results are probably caused by clinically available tests that do not exactly reflect Eustachian tube function under normal physiological conditions. Although only the Valsalva maneuver test was used to measure subjective Eustachian tube function in this study, a more exact evaluation could be explored if the results of objective tests such as manometry are added.
Preoperative ABG was significantly smaller in the otorrhea group than that in non-otorrhea group in this study. The difference in postoperative ABG between these two groups seemed to get smaller as mucosal status gradually improved after surgery, suggesting that decreased bone conduction hearing can be caused by poor mucosal status in patients with otorrhea.9) Further studies should be conducted for an exact explanation.
Pre and postoperative ABGs according to the size of the tympanic membrane perforation showed that the hearing improvement was smaller in patients with a Griffin grade I perforation than in those with Griffin grades II or III perforations. This was likely due to the fact that conductive hearing loss worsens as a tympanic membrane perforation becomes larger.
Hearing levels varied in previous studies based on preoperative ossicular chain destruction.15,16) Furthermore, the difference in hearing levels also vary due to differences in the classification system of the ossicular chain destruction used. Iurato, et al.17) graded the severity of ossicular injuries into four subclasses based on the presence of the malleus and stapes. Five degrees of ossicular injury severity were identified based on integrity of the main joints, such as the malleolar-incudial and the incudo-stapedial joint, in this study. This method has the advantage of planning step-by-step surgery from preoperative 3D CT, which can provide imaging data that more closely visualizes ossicular status. If the ossicular chain is injured, it should be artificially reconstructed. When ossicular implants are used, the lever action observed in the normal ossicular chain will be lost. Placing an implant between the malleus and stapes produces better results (<20 dB of ABG) compared to cases in which ossicular implants directly contact the tympanic membrane.18) Thus, ossicular implants should be located between the malleus and the stapes as much as possible. In particular, the ossicular chain should be reconstructed on the stapes footplate for hearing improvement in cases of a destroyed stapes supra-structure. As there is a higher risk of ossicular sliding when the ossicular implant is directly positioned on the stapes footplate, hearing improvement is reportedly poorer due to the unstable ossicular chain than when the ossicular implant is positioned over the stapes head.19) In this study, interpositioning or a columella over the stapes head (Si or Sc) was performed in cases of intact stapes supra-structure, and interpositioning or a columella over the stapedial footplate (Fi or Fc) was performed in cases of an injured stapes suprastructure. Poorer hearing improvement after the surgery in patients with an injured stapes supra-structure in this study was consistent with the results of a previous study.8)
The results of this study showed poorer hearing improvement in the cholesteatoma group than that in the noncholesteatoma group, which was also consistent with the results of previous studies. In particular, the poorest hearing improvement was observed in cases of tensa cholesteatoma.15) This is likely because a cholesteatoma with inflammation propagates more easily to adjacent important hearing structures, such as the stapes. Furthermore, inflammatory tissues of the round window and the oval window require excessive manipulation of the stapes to remove lesions.18) Another reason is that ossiculoplasty to improve hearing is more difficult, because patients with a cholesteatoma often have more severe ossicular injuries.15) Complete removal of disease is often more important as a purpose for cholesteatoma surgery than hearing improvement. Thus, postoperative hearing improvement is likely to be poorer in patients with a cholesteatoma than those without.
Changes in postoperative hearing level may vary depending on the skill of the surgeon performing the ossiculoplasty and the materials used. As this study focused on the overall hearing threshold changes after surgery, detailed surgical techniques and kinds of prostheses with their success rate are left for further study.
Paparella, et al.9) reported that toxic substances and by-products of the inflammatory response pass through the round window and cause biochemical changes in the endocochlear lymph fluid in patients with COM, which leads to sensorineural hearing loss in almost all frequency bands. They also noticed that bone conduction hearing was poorer in cases of poor middle ear mucosal status, as English, et al.10) reported. The results of this study also showed that the hearing improvement after ossiculoplasty was poorer in patients with COM than in nonCOM cases. However it could not be ruled out that the results could have been influenced by drilling or other manipulations during the mastoidectomy. Therefore, it is difficult to conclude that the inflammatory lesions in the middle ear alone affect hearing outcomes after surgery.20)
The results of this relatively large scale study of COM surgery conducted by a single surgeon are meaningful, because it provided reliable results by minimizing the confounding variables caused by variability in surgeon performance and experience together with a brief review and summary of previous studies using various methods.
Conclusion
The effects of middle ear lesions on pre and postoperative hearing were investigated using more than 2000 COM surgical records retrieved from a middle ear surgery computerized database, which was released by the Korean Otologic Society in 2005. Preoperative hearing was poor in patients with Eustachian tube dysfunction, cholesteatoma, and a tensa type of cholesteatoma. The postoperative hearing gain was poorer in patients with a destroyed stapes than in those with other ossicle problems, although preoperative hearing levels were not different among them.
The postoperative hearing gains were also poor in patients with middle ear lesions such as tensa type cholesteatoma, the presence of inflammation, large tympanic membrane perforations, and Eustachian tube dysfunction. The results of this study will be useful for designing future clinical studies on middle ear surgery, as well as for surgical planning and patient counseling in clinical practice.