Nasal Colonization of Methicillin-Resistant Staphylococcus aureus in Patients with Chronic Suppurative Otitis Media
Article information
Abstract
Background and Objectives
Methicillin-resistant Staphylococcus aureus (MRSA) is one of major pathogens in patients with chronic suppurative otitis media (CSOM). In addition to intrinsic MRSA infection of the mastoid air cell system, nasal colonization of MRSA, a known predictor of postoperative surgical site infection, may pose increased risk of postoperative complications. The purpose of this study is to describe microbiology of preoperative nasal swab screening and localized middle ear specimens in patients undergoing otologic surgeries.
Subjects and Methods
Forty-nine consecutive patients with CSOM who underwent middle ear surgery were included. Preoperative nasal swabs for MRSA, and preoperative and intraoperative middle ear swabs were collected and compared for pathogens.
Results
Preoperative nasal swab screening confirmed MRSA colonization in 3/49 patients (6.1%) and methicillin-resistant coagulase-negative Staphylococcus (MRCNS) in 9/49 patients (18.4%). Correlation with preoperative culture results and nasal swab screening results were compatible in 2/4 patients with positive nasal swab for MRSA and 1/9 patients with positive nasal swab for MRCNS. Postoperative conversion to MRSA was observed in 3 patients.
Conclusions
The rate of nasal MRSA colonization among patients with CSOM was higher than among the general community. Preoperative MRSA colonization was associated with MRSA from middle ear specimens. Further studies are warranted to investigate the possible benefit of preoperative treatment of MRSA colonized patients undergoing middle ear surgeries.
Introduction
Chronic suppurative otitis media (CSOM) is an inflammatory disease of the middle ear and mastoid air cell system, which can result in irreversible changes not only in the middle ear structures but also in the inner ear.1) Dysfunction of the Eustachian tube and the bacterial infection are important factors in the multifactorial pathogenesis of CSOM. In order to eradicate inflammation, prevent recurrence and restore middle ear structures and hearing, both medical and surgical treatment modalities are important in CSOM. It has been emphasized that selection of appropriate antibiotics should be based on the bacteriologic studies to identify the pathogens and determine sensitivities.2,3)
Recent bacteriologic studies of the middle ear discharge in CSOM in Korea have reported increasing prevalence of methicillin-resistant Staphylococcus aureus (MRSA).2,4,5) In addition, Staphylococcus aureus (S. aureus) and Pseudomonas species were most predominant from the postoperative otorrhea cultures.3) Higher rates of postoperative otorrhea and reperforation after tympanomastoid surgeries were reported in CSOM patients with MRSA cultured from preoperative ear discharge.6)
In addition to intrinsic MRSA infection of the mastoid air cell system, nasal colonization of MRSA may pose increased risk of postoperative infection. Nasal colonization rate of MRSA and it is a known predictor of postoperative surgical site infection.7,8) Previous studies have identified bacterial pathogens from the middle ear and the mastoid air cells, or nasopharynx as a bacterial reservoir in CSOM.4,5,9-12)
However, few studies have focused on the effect of nasal MRSA colonization in the otologic surgery. The aims of this study are to examine the prevalence of nasal MRSA colonization in patients undergoing otologic surgeries and to determine the association between MRSA colonization and the pathogens identified from perioperative culture studies.
Subjects and Methods
The study included 66 consecutive patients (25 males and 41 females) undergoing tympanomastoid surgeries from May 2010 to December 2011 at the Yonsei University College of Medicine Gangnam Severance Hospital. Patients with intracranial or extratemporal complications of CSOM, known history of external radiation, known history of corticosteroid therapy preoperatively, or those undergoing emergency operations were excluded. The mean age at operation was 51.7±15.7 years (range 34-74 years), and the right ear was operated in 34 ears, the left in 32 ears.
Upon the initial visit in the outpatient department, the external auditory canal was cleaned, and the middle ear discharge was collected with collected with cotton swabs through sterile otoscopes, taking care not to touch the external auditory canal skin. To assess nasal colonization of S. aureus, a nasal swab was taken before the operation in addition to routine preoperative testing. The nasal samples were obtained by cotton swab from the anterior vestibular of the nares by the physician. During the operation, intraoperative culture specimens were taken in cases with overt discharge in the middle ear cavity. During postoperative period of 1 month, postoperative culture specimens were again taken in cases with otorrhea through the external auditory canal. All culture samples were in Stuart transport medium and transported to the laboratory, where the samples were inoculated onto blood agar, MacConkey's agar, and chocolate agar plates. All plates were incubated at 37-C aerobically under 5% (v/v) CO2 and examined 24 and 48 hours later. Bacteria were identified morphologically using Gram staining and biochemically. Susceptibility testing was performed using disk diffusion. Identified pathogen species and antimicrobial susceptibility were compared between nasal swab and perioperative (preoperative, intraoperative and postoperative otorrhea) cultures. Statistical analysis was performed with Fisher's exact testusing SPSS statistical software (version 15.0; SPSS Inc., Chicago, IL, USA). The criterion for statistical significance was p<0.05.
Results
Among the 67 patients undergoing operation for CSOM, nasal swab confirmed bacterial colonization in 37 (55.2%) patients (Table 1). Clinically importantly, nasal cavity colonization of S. aureus was noted in 10/67 (14.9%) of patients, and 4/67 (6.0%) patients were positive for MRSA. Also, methicillin-sensitive Staphylococcus aureus (MSSA) was identified in 9/37 (23.4%) and methicillin-resistant coagulase-negative Staphylococcus (MRCNS) in 11/67 (13.4%) of patients. Preoperative ear culture studies identified pathogens in 39/67 (58.2%) of the patients: the most commonly identified species was Staphylococcus [MRCNS 26.9%, methicillin-sensitive coagulase-negative Staphylococcus (MSCNS) 1.5%, MRSA 13.4% and MSSA 11.9%]. Intraoperatively, overt discharge from the middle ear mucosa was noted in 40 ears. Most of the intraoperative culture results were negative (28/40 ears, 71.8%). MRSA was found in 3/40 (4.5%) ears, MSSA in 2 ears (3.0%), MRCNS in 2 ears (3.0%) and MSCNS in 1 ear (1.5%). After the surgery, 11 of the 67 patients developed otorrhea within 1 month postoperatively. The postoperative culture studies identified MRSA in 3/11 (27.3%) and Acinetobacter species in 1/11 (9.1%) and fungus in 2/11 (18.1%) patients (Table 2). No pathogens were identified in the remaining 5 patients (45.5%).
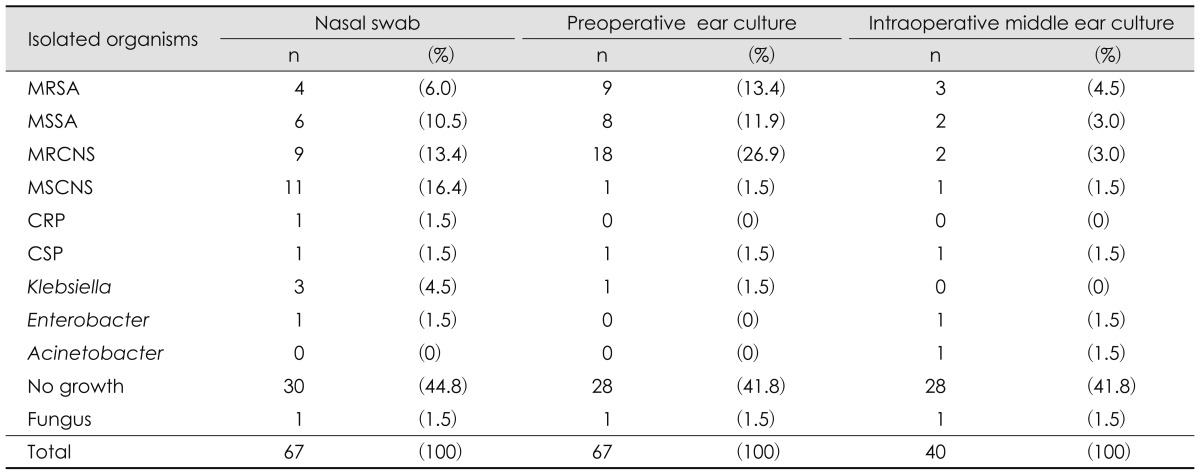
Organisms identified from nasal swabs, compared to the preoperative otorrhea, intraoperative middle ear culture results
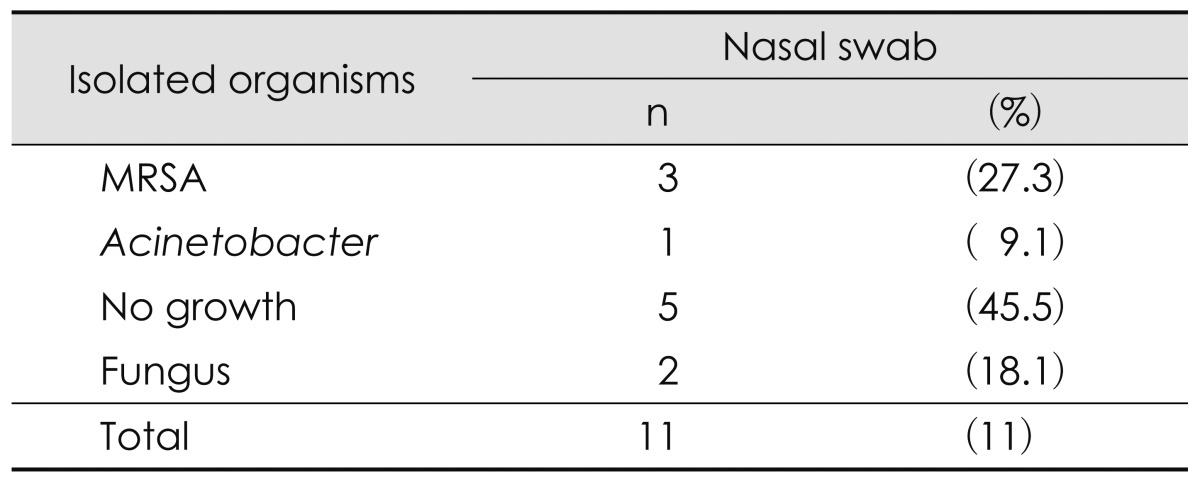
Organisms identified from postoperative otorrhea cultures from 11 patients that developed postoperative infection
The isolated organisms were compared between the nasal swab and perioperative cultures (Fig. 1). Preoperative ear culture results and nasal swab culture results showed significant difference (p=0.001), as well as intraoperative middle ear cultures and postoperative otorrhea culture results showed significant difference (p=0.023). However, no significant difference was noted between preoperative ear and postoperative otorrhea culture results (p=0.493). Then we compared the culture results according to the presence of bacterial growth and reports of no growth (Fig. 2). No significant difference was noted between preoperative ear culture, and nasal swab culture results (p=0.055), between preoperative ear and postoperative otorrhea culture results (p=0.068), or nasal swab and postoperative otorrhea culture results (p=0.094). Lastly, the culture results were compared according to the presence of antibiotic resistance (Fig. 3). No significant difference was noted between the antibiotic-susceptible and resistant strains identified between preoperative ear culture and nasal swab cultures (p=0.098), or between preoperative ear and postoperative otorrhea cultures (p=0.053).
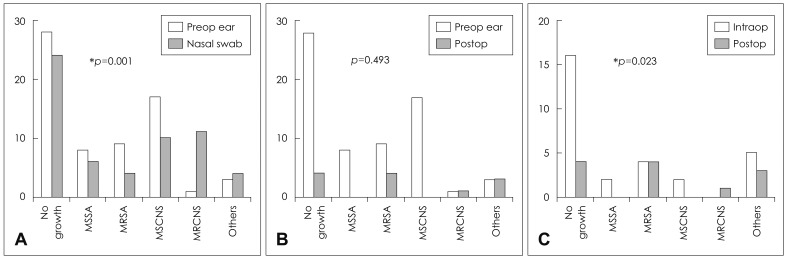
Comparison of organisms identified from perioperative cultures and nasal swab. (A) Preoperative ear culture results (Preop ear) and nasal swab (Nasal) culture results showed significant difference (p=0.001). However, no significant correlation was noted between Preop ear and postoperative (Postop) culture results (B). (C) Intraoperative middle ear cultures (Intraop) and Postop culture results showed significant difference (p=0.023). *p<0.05.
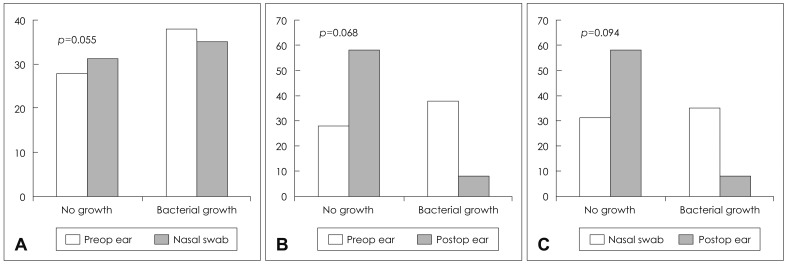
Comparison of culture results according to the presence of bacterial growth. No significant difference was noted between the presence of bacterial growth or no growth when the culture results were compared: (A) preoperative ear culture (Preop ear), and nasal swab (Nasal), (B) Preop ear and postoperative (Postop) culture, or (C) Nasal and Postop.
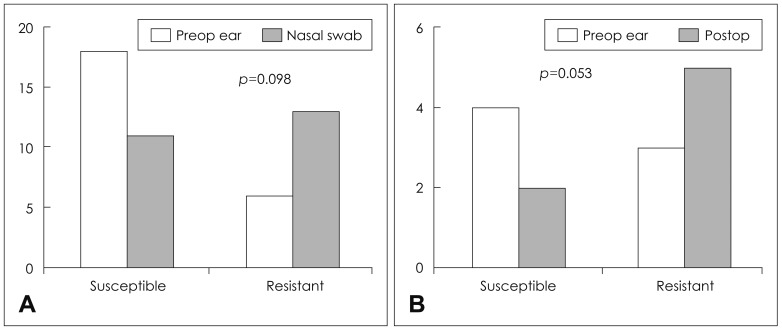
Comparison of culture results according to the presence of antibiotic resistance. No significant difference was noted between the antibiotic-susceptible and resistant strains identified when the culture results were compared between (A) preoperative ear culture (Preop ear), and nasal swab (Nasal), (B) Preop ear and postoperative (Postop) culture.
Then we analyzed the correlation of isolated organisms from the nasal swab and other cultures in patients with nasal colonization of antibiotic-resistant strains (Fig. 4). Among 4 patients with identified with nasal MRSA colonization, preoperative ear cultures were also positive for MRSA in 3 patients (75.0%). However, intraoperative culture identified MRSA in only one patient, and none of the patients developed MRSA infection postoperatively. Twelve patients were identified with nasal MRCNS colonization. Preoperative ear cultures reported MRSA in 1, MRCNS in 1, and MSCNS in 7, ciprobay-resistant Pseudomonas in 1, and no growth in 2 patients. MRCNS was identified from intraoperative culture in only 1 patient. Again, only 1 patient developed otorrhea due to MRSA in the postoperative period.

Diagram to show the analysis of the perioperative culture results from the patients identified with nasal MRSA or MRCNS colonization. MRSA: methicillin-resistant Staphylococcus aureus, MRCNS: methicillin-resistant coagulase-negative Staphylococcus, MSCNS: methicillin-sensitive coagulase-negative Staphylococcus, CRP: ciprobay-resistant Pseudomonas.
Discussion
Staphylococcus and Pseudomonas species are most frequent pathogens in CSOM. Increasing incidence of antibiotic-resistant bacterial strains in CSOM patients poses a challenge to not only the selection of appropriate antibiotics therapy, but also to prevent the emergence of resistance to glycopeptides, the main drugs chosen for MRSA. It has been reported that patients who are colonized with S. aureus are the main source of S. aureus in hospitals, and that nasal carriage of MRSA increases the risk of postoperative infection. Since the rate of methicillin resistance is higher in Korean CSOM patients compared to other countries, we examined the rate of nasal MRSA colonization. The rate of nasal carriage of MRSA in CSOM patients was higher than among healthy individuals reported as 0.2-2.8% of the United States population.7) Although this study was limited to small number of patients, the finding may suggest that in addition to nosocomial infection, community-acquired MRSA infection may contribute partially to the relatively higher rate of MRSA in CSOM patients in Korea. On the other hand, the rates of bacterial isolation from preoperative ear discharge, intraoperative middle ear discharge, or postoperative otorrhea cultures in our patients were lower. Also, the perioperative culture studies frequently reported no growth of pathogens. Given that the patients were prescribed with antibiotics prior to surgery, it may signify that current antibiotics are effective in infection control during the tympanomastoid surgery. Furthermore, the interpretation of the culture results from postoperative otorrhea is limited since antibiotics were routinely used postoperatively in all patients and culture samples were taken from the external auditory canal in cases with overt otorrhea or from wet surface of the grafted tympanic membrane immediately after removal of the packing material at 2 weeks postoperatively. The culture results can only reflect that MRSA infection that could not be controlled by routine antibiotics, which may be clinically significant.
MRSA is a common pathogen in otologic diseases. MRSA has been identified not only in CSOM patients,2,3,5,13) but also in patients with external otitis.14) S. aureus has been implicated in biofilm formation complicating cochlear implants.15-17) Nasal MRSA colonization deserves attention since transmission from nasal carriage to surgical site infections or bacteremia is possible, and it is associated with increased morbidity and mortality. Previous studies have reported that elimination of nasal MRSA colonization reduces the risk of postoperative infections.8,18,19) Application of 2% mupirocin calcium ointment to the nares has been proven to be effective, and chlorhexidine-based solutions is used to reduce the density of skin colonization of MRSA preoperatively.18-20) A recent study compared the rates of MRSA infection in otolaryngology surgeries, before and after implementation of preoperative screening and treatment of nasal MRSA carriage.21) Further studies are warranted to investigate the possible benefit of preoperative treatment of MRSA colonized patients undergoing middle ear surgeries.
Conclusion
The rate of nasal MRSA colonization among patients with CSOM was higher than among the general community. Preoperative MRSA colonization was associated with MRSA from middle ear specimens. Further studies are warranted to investigate the possible benefit of preoperative treatment of MRSA colonized patients undergoing middle ear surgeries.