Clinical and Social Outcomes of Cochlear Implantation in Older Prelinguals
Article information
Abstract
Background and Objectives
Cochlear implantation in late implanted prelinguals necessitates a complex decision-making process for clinicians and patients due to the uncertainty of achieving adequate benefit in auditory and speech perception. This study longitudinally evaluated clinical and social outcomes of prelingually deaf children with implantation in their late childhood.
Subjects and Methods
A total of 113 (49 females and 64 males) participants, with an age range of 5-15 years, were assessed for the pre-implant parameters such as hearing loss etiology, aided responses, anatomical aspects, and psychological evaluation. The Category of Auditory Performance, Speech Awareness Threshold, Speech Reception Threshold, and Speech Discrimination Score were administered to assess the patient’s auditory skills. Further, the Speech Intelligibility Rating scale was administered to evaluate the patient’s speech intelligibility at 3, 6, 9, 12, 18, and 24 months post-surgery. Subjectively perceived benefits were evaluated using the satisfaction rating scale and a questionnaire.
Results
The statistical results showed a significant impact of cochlear implantation in all domains. Positive impact and improvement post-implantation were noted in all the spheres, including auditory, linguistic, social, and educational.
Conclusions
The study highlighted that the outcomes of a cochlear implant at a later age might not parallel with the implantation at a younger age. However, this still provides measurable benefits even after a longer period of auditory deprivation.
Introduction
Congenital hearing impairment affects the development of children in more than one domain with major impact on speech and language skills. They require intervention as early as possible and in cases of no benefit from conventional hearing aids, the cochlear implants (CIs) have proven to be the most reliable rehabilitative measure [1] with significant improvement in speech comprehension and expression [2] and reading skills [3]. Among the children implanted with CIs, the speech and language outcomes are highly variable and are influenced by several factors including age at onset of deafness, duration of profound deafness, communication mode, pre-operative residual hearing, and nonverbal cognition [4-6]. Among these, the advanced age at implantation is detrimental in restoring normal auditory processing function. The length of deafness prior to receiving a CI has been reported to be negatively connected with the ability to comprehend and employ verbal-linguistic skills [7]. If the targets of early hearing detection and interventions are met such as hearing screening by 1 month, confirmation by 3 months, and intervention by 9 months, the speech and language skills of child with hearing loss can be at par with their normal hearing counterparts [8].
Every neonate in the United States gets evaluated for hearing impairment prior to discharge because of the implementation of a universal newborn hearing screening programe [9]. In contrast, in developing countries such as India, hearing loss is often detected by parents, resulting in a significant delay in auditory rehabilitation. Hearing loss is discovered at mean age of 3.03 years in eastern India [10] with mean implantation age of 4.79 years [11] and subsequent aural rehabilitation much delayed. Cochlear implantation in this group of patients necessitates a difficult decision-making process for both clinicians and patients due to the uncertainty of achieving adequate benefits in auditory and speech perception abilities [12]. Several studies have shown that the CI could significantly improve speech perception in this group of patients [13]. However, factors such as the cause of hearing loss, manner of communication, educational status, and attendance at speech therapy sessions may all have an impact on post-implant outcomes and needs investigation. Therefore, the purpose of this study was to determine the long-term speech and language outcomes, assessment of hearing abilities, and self-perceived benefits of CI in children with prelingual deafness and late implantation.
Subjects and Methods
This descriptive longitudinal observational study included children with prelingually bilateral severe to profound sensorineural hearing loss who underwent cochlear implantation at ≥5 years of age from September 2001 to July 2021 at the institute. All the participants received unilateral implant with 102 implanted on right side and 11 on left side. Both retrospective (n=70) and prospective (n=43) subjects were included. Children with unilateral hearing loss, auditory neuropathy spectrum disorder, intellectual deficits, attention deficits, and neuromuscular deficits were excluded. A written informed consent was obtained from the all parents and institutional ethical committee clearance was obtained for the study (IEC-23/04.01.2019).
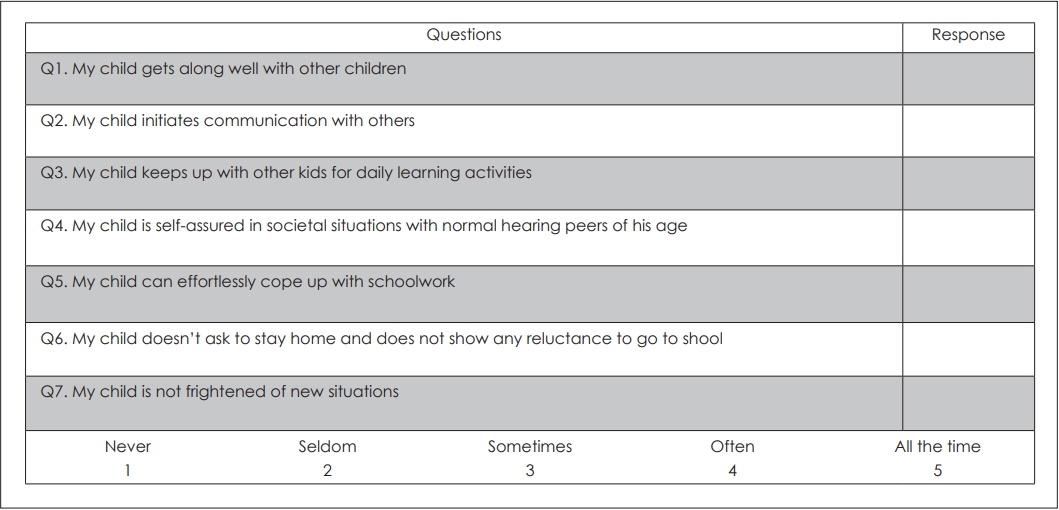
Relevant information such as details of hearing loss, demographic details, medical history, family history, socioeconomic background, language exposure, and outcomes of various measures were recorded. To determine the socioeconomic status (SES) of the subjects, modified Kuppuswamy socioeconomic scale [14] was used. Various scales and tests were used to measure the outcomes. The auditory abilities were examined using Categories of Auditory Performance (CAP). Speech Awareness Threshold (SAT), Speech Recognition Thresholds (SRT), and Speech Discrimination Score (SDS) were used to record the speech perception abilities. The Speech Intelligibility Rating (SIR) was used to assess the intelligibility of speech in everyday spontaneous verbal communication. Pre- and post-implant educational set up was also studied to see the impact of CI on educational profile. Subjectively perceived benefits were evaluated using the satisfaction rating scale of 0-10 with 0 being the least and 10 being maximum. The social impact on child from parent’s perspective was investigated using a structured set of seven questions related to social communicative behaviour with Likert scale. Parents were asked to state their level of accord with every statement on a scale of 1-5 as shown in Fig. 1.
A follow-up was carried out at regular intervals of 3, 6, 12, 18, and 24 months with minimum and maximum follow-up of 3 months and 237 months, respectively, and median follow-up of 31 months. All the details and scores obtained were tabulated in Microsoft Excel and analyzed. Data were analyzed by using statistical software Stata 14.0 (StataCorp, College Station, TX, USA). Categorical data were expressed as frequency and percentage. Quantitative data were expressed as mean and standard deviation, median and interquartile range. Kruskal-Wallis H test was used to compare scores among the SES categories. Mann-Whitney U test was used to compare scores between languages wherein p<0.05 was considered as statistically significant.
Results
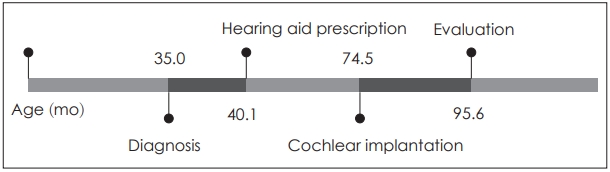
A total of 113 (64 males and 49 females) children with CI in late childhood were included with age range of 5-15 years (mean age: 7.97±2.8 years). Relevant case history and possible etiology of hearing impairment were assessed based on available medical documents and patient interview. The age of diagnosis of hearing loss ranged from 6 to 66 months (mean±SD; 35±12.9 months), age of hearing aid prescription ranged from 7 to 72 months (mean age: 40.1±13.2 months) and age of cochlear implantation ranged from 60 to 144 months (mean age 74.5±17 months). The timeline of events for the subjects is summarized in Fig. 2.
Out of 113 subjects, 109 were hearing aid users whereas 4 were nonusers. A total of 103 subjects started using hearing aids within 6 months and 6 subjects within 12 months of prescribing the aids. Radiological abnormalities, intraoperative complications, and intraoperative electrically evoked compound action potential (ECAP) responses were noted. Socioeconomic background based on the Modified Kuppuswamy socioeconomic scale and language exposure were also assessed as illustrated in Table 1.
Assessment of auditory and speech skills
Both pre- and post-implant CAP scores were obtained. The CAP scores before the implantation ranged from 0 to 4 with the median value of 1. Compared to this, post-implantation best scores ranged from 1 to 7 with the median value of 5 (p<0.0001). Follow-up was done at regular intervals and CAP scores were noted to improve at 3 months post-implantation, saturating at around 24 months. A cross-sectional view of average CAP scores over the period after implantation is summarized in Fig. 3A.
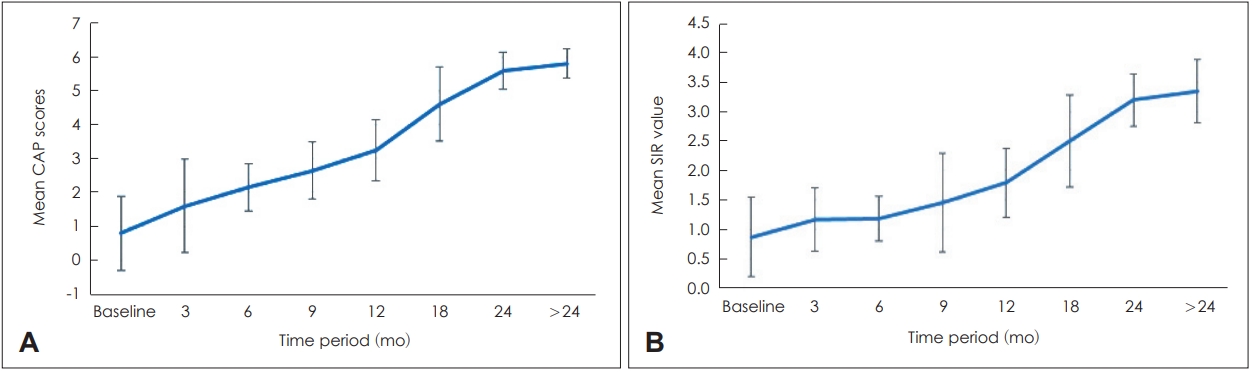
Averaged post-implant CAP (A) and SIR (B) scores over the period. CAP, Categories of Auditory Performance; SIR, Speech Intelligibility Rating.
The pre-implant and post-implant SIR scores were obtained in all the subjects. Pre-implant SIR scores in 113 subjects ranged from 1 to 3 (mean score 1) that increased to 1 to 5 (mean score 3) post-implantation (p>0.05). The SIR score was measured serially in post-implantation follow-up visits at regular intervals and the average values obtained for the cohort at various time points are shown in Fig. 3B.
Pre- and post-implant SAT were assessed. Mean pre-implant threshold was found to be 73 dB with hearing aids and post-implantation it was reported to be 45 dB. To assess the auditory recognition skills pre- and post-implantation SRT and SDS were recorded. The SRT levels in the pre-implantation period could not be assessed in 105 subjects due to inadequate speech and language skills and no benefit from hearing aids. For those with some benefit with hearing aids, aided SRT was noted to be 76 dB. Post-implant SRT was obtained for only 87 subjects due to very poor speech discrimination or lack of reliable physical follow-up. In 87 subjects mean SRT was found to be 58.9 dB. Same as SRT, pre-implant SDS could not be assessed in 107 subjects due to inadequate skills. In 7 subjects with minimal benefit with hearing aids closed set, mean SDS was found to be 15%. Post-implant closed set SDS was recorded for 90 subjects with mean score of 79%.
Mode of communication and social communicative behaviour
Pre-implant and post-implant predominant mode of communication was recorded to see the impact on communicative profile. Before surgery, 81% were using manual mode of communication and 4.4% were using oral mode of communication. Whereas 35% moved to oral mode of communication and 63.5% relied on total communication post-implantation. Also, the communicative mode opted by primary caregiver was recorded. Only 11% caregivers were using spoken language before CI that increased to 50.44% after implantation.
The pre- and post-implant impact on social behavior was assessed with a set of seven questions (Fig. 1). Scores obtained in all seven questions were averaged separately post-implantation and compared with the scores pre-implantation period for all the subjects as shown in Fig. 4. The average scores for all the questions increased from pre-implantation 2 (SD, ±1) to post-implantation period 4 (SD, ±1) (p<0.001) as depicted in Table 2.
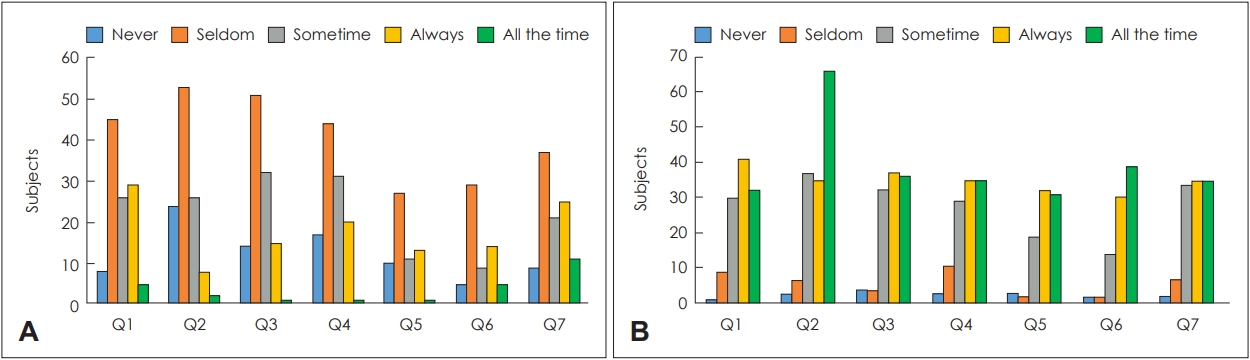
Responses to social communication questionnaires. A: Pre-implantation questionnaire response. B: Post-implantation questionnaire response.
Educational profile and satisfaction rating
The pre- and post-implant educational profiles of subjects were assessed by comparing the opted educational setup. Of the total subjects, 53.6% had enrolled in educational setup whereas post implantation this increased to 75.8%. With respect to mainstream education, 49.4% of the subjects were attending mainstream education pre-implantation and this increased to 70.6% post-implantation. The remaining were enrolled in segregated or integrated educational setup and did not show major variation in pre- and post-implant condition.
Satisfaction among the caregiver with CI was considered as an important outcome parameter. Pre- and post-implant parental satisfaction was measured and on a scale of 0-10, pre-implantation median score was 1 whereas post-implantation this improved to 8 and the difference was found to be statistically significant (p<0.0001).
Hearing aid usage and auditory training
In pre-implantation period, a total of 108 were using hearing aids. This number decreased to 106 post-implantations with CIs. Therefore, the number of subjects using the device showed slight decrease. However, the daily usage of CI device showed improvement with 96 subjects using the implant device for 10.1-15 hours per day whereas hearing aids were used for 10.1-15 hours by only 40 subjects as shown in Fig. 5.
Auditory training schedule of the subjects in pre-implantation and post-implantation period was assessed. The auditor-yverbal therapy sessions were taken by 84 out of 113 in pre-implantation period with hearing aids that increased to 92 post-implantation with CIs. However, the number of sessions requested by parents per week and their physical attendance for these sessions reduced significantly post-implantation from 80% to 60% due to traveling constraints and preference for teleconsultation.
Effect of SES and language exposure on SIR and CAP scores
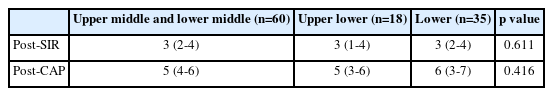
The effects of SES and language exposure on auditory and speech outcomes, i.e., CAP and SIR, were also assessed in implantees. The upper-middle and lower-middle classes were analyzed together due to a smaller number of subjects in upper-middle category. The post-SIR and post-CAP scores were not statistically significant among the three SES categories (p=0.611 and p=0.416, respectively) and improvement was observed across all the categories post-implantation as shown in Table 3.
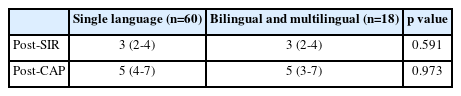
Similarly, effect of language outcome was assessed wherein the bilingual and multilingual categories were analyzed together due to a smaller number of subjects in multilingual category. The post-SIR and post-CAP scores were not statistically significant among the three language categories (p=0.591 and p=0.973, respectively) and improvement was observed across all the categories post-implantation as shown in Table 4.
Discussion
The available literature suggests that prelingual deaf children who undergo cochlear implantation at age less than three years perform better in terms of auditory, speech, and language outcomes [15-17]. However, this is a rare scenario in developing nations like the Indian subcontinent. A study performed previously at our institute reported the mean age at implantation to be 4.79 years [13]. Therefore, the outcomes in these children cannot be generalized to the ones with traditionally recommended age of implantation, as there are several factors that can affect their performances. In India where the implantation often takes place at a later age, it becomes crucial to study these factors and their effect on hearing and language abilities in these children.
In the present study, the mean age of implantation was 6.2 years. Hearing impairment was reported to be idiopathic for most of the patients during the pre-implant evaluation. The Joint Committee of Infant Hearing has identified several factors causing hearing loss, with positive family history [18] being one of the most significant risk factors followed by the syndromes [19] and infections such as cytomegalovirus [20]. However, in the current study, these had little contribution.
The surgery-related factors such as anatomical malformations and intraoperative complications were negligible. The longer duration of device use post-surgery was prevalent in the present cohort with 96 out of 113 using the device for 10-15 hours each day. The consistency for therapy sessions before and after CI surgery did not show much improvement which could be attributed to pandemic-associated restrictions. Also, the impact of the SES of parents and language exposure at home of all the subjects were evaluated. In a study from southern India by Merugumala, et al. [21] that aimed to investigate the barriers to early diagnosis of hearing impairment in India, low socioeconomic backgrounds and consequently lack of timely screening was found to affect the early detection and treatment of hearing impairment. In the current research, 96% of the subjects were from middle or lower socioeconomic background that might have contributed to the delayed rehabilitation of these children due to lack of awareness and financial constraints. On assessing the effect of socioeconomic background and language exposure on CAP and SIR scores, it was found that both had equal effect across the categories on auditory and speech outcomes post-implantation and was not statistically significant suggesting that irrespective of SES category and type of language exposure at home, all the subjects in the current study showed improvement in CAP and SIR scores post-implantation.
The CAP and SIR scores were primary criteria for assessment in our study. The late implantees in the current research attained a median CAP and SIR score of 5 and 3, respectively, at 24 months indicating that they are able to understand common phrases without lip reading and connected speech is not unintelligible. Although these are not the maximum possible outcomes, they are not ignorable and can significantly augment the daily life of prelingually deaf child. In a study by Fang, et al. [22], auditory performance (CAP score) and speech intelligibility (SIR) of 84 early implanted prelingually deaf children were recorded post-implantation for 1, 2, 3, 4, and 5 years. The study reported the median CAP score to be 5 and attaining plateau after 24 months of implant use. The median SIR was reported to be 3 and it attained the maximum outcome after 24 months of device use. In the present study, the median of CAP and SIR scores obtained post-implantation were tabulated against the scores at similar interval from the literature [22] recorded for early implanted prelinguals. The median CAP and SIR scores of the patients are summarized in Fig. 6A and B, respectively.

Median CAP (A) and SIR (B) scores at regular intervals for late and early implanted prelinguals. CAP, Categories of Auditory Performance; SIR, Speech Intelligibility Rating.
As expected, the median CAP and SIR of early implanted prelinguals were better at 12 months and 24 months as compared to the scores of late implanted prelinguals. The median CAP score at 12 months, of early implanted prelinguals was reported to be 4, whereas for the late prelinguals it was observed to be 3. Similarly, SIR score at 12 months for early implanted prelinguals was 2 and it further progressed to 3 at 24 months. However, in case of late implanted prelinguals, the median SIR score was observed to be 2 at 12 months and it attained a plateau of 2.4 at 24 months. Also, a statistically significant improvement was observed in CAP and SIR scores obtained after implantation as compared to the ones recorded before implantation. These results suggest that the performance on CAP and SIR scale is affected by the age of implantation and is better in early implanted as compared to the late implanted individuals. It progresses at faster pace in case of early implanted children with hearing impairment as compared to the late implanted subjects. However, after implantation, a definite improvement in the scores is noted in late implanted prelinguals as well. The mean SAT improved from 73 dB before implantation to 45 dB after implantation as did the mean SRT and mean SDS scores that increased from 76 dB to 58 dB, and 15% to 79%, respectively. These results indicate overall improvement in auditory awareness skills in the targeted population.
Another factor that this study aimed to study was to ascertain parental/caregiver satisfaction with the CIs. Along with the restoration of hearing abilities, cochlear implantation also helps the child to adapt to the immediate environment such as home, school, and society and further improves the quality of life of the child. Wheeler, et al. [23] had reported that the shift from sign language to total or completely oral mode of communication in 11 out of 12 of their subjects after the implantation. Parents play a decisive role in this rehabilitation process. Rout and Khanna [24] investigated the key concerns of mothers regarding the needs and difficulties faced by the child with hearing impairment and reinforced on the need of language and cultural directed materials to address the parental concerns. In our study, a 10-point parental satisfaction scale and a questionnaire was administered. The median parental satisfaction score improved to 8 post-surgery which was recorded to be 1 before implantation. Most of the parents were satisfied with children’s auditory abilities after the cochlear implantation. The questionnaire comprising of seven questions to assess the subject’s communication abilities among peer groups and at school was administered. Majority of the parents rated the performance of their children 4 or 5 on a 5-point rating scale after the implantation indicating improved communication skills of the subjects while interacting with the peer group and at the school.
The ambispective analysis of our study concluded that the delayed intervention with cochlear implantation in prelingual children can result in improvement in all domains including auditory behavior and language skills. In a prospective study by Kos, et al. [25], the late implanted subjects showed improved awareness of oral language structures and better performance on CAP and SIR. Similarly, Liu, et al. [26] reported the speech assessment of retrospectively studied group of 94 late implanted prelingual subjects. The study stated that cochlear implantation in late prelinguals is an effective intervention option but can take a longer duration for rehabilitation compared to their early implanted counterparts. Therefore, cochlear implantation in late prelinguals is a viable option and should be considered along with intensive post-implantation speech and language rehabilitation.
The present study explored the clinico-social outcomes of cochlear implantation in children with severe to profound prelingual deafness who underwent cochlear implantation later than recommended age of implantation. The findings indicated that the outcomes with CI at the later age may not parallel with the implantation at younger age, but it still provides measurable benefits even after longer period of auditory deprivation. These findings should encourage the concerned authorities and funding agencies in the country to extend the support for select groups of these children who have not been able to get the benefits of implantation at an early age. Thorough evaluation of such patients and due recommendations by board of experts are however strongly recommended. Also, future studies can be carried out by employing dual arm analysis within a demographically more comparable patient cohort.
Acknowledgements
The Cochlear Implant Group of India (CIGI)—funding agency. The Research Section, All India Institute of Medical Sciences (New Delhi).
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Kapil Sikka, Alok Thakar. Data curation: Tanvi Chaudhary, Sonam Sharma, Divya Chauhan. Formal analysis: Divya Chauhan, Mayank Bhutada, Pragya Tyagi. Funding acquisition: Kapil Sikka. Investigation: Tanvi Chaudhary, Sonam Sharma, Divya Chauhan, Shivani Agarwal, Anup Singh. Methodology: Tanvi Chaudhary, Kapil Sikka. Project administration: Kapil Sikka. Supervision: Alok Thakar, Rakesh Kumar, Prem Sagar, Hitesh Verma. Writing—original draft: Divya Chauhan, Pragya Tyagi. Writing—review & editing: Kapil Sikka, Anup Singh, Divya Chauhan, Pragya Tyagi. Approval of final manuscript: all authors.