|
 |
- Search
| J Audiol Otol > Volume 19(1); 2015 > Article |
|
Abstract
Background and Objectives
To evaluate the relationship between age and anesthesia method used for tympanostomy tube insertion (TTI) and to provide evidence to guide the selection of an appropriate anesthesia method in children.
Subjects and Methods
We performed a retrospective review of children under 15 years of age who underwent tympanostomy tube insertion (n=159) or myringotomy alone (n=175) under local or general anesthesia by a single surgeon at a university-based, secondary care referral hospital. Epidermiologic data between local and general anesthesia groups as well as between TTI and myringotomy were analyzed. Medical costs were compared between local and general anesthesia groups.
Results
Children who received local anesthesia were significantly older than those who received general anesthesia. Unilateral tympanostomy tube insertion was performed more frequently under local anesthesia than bilateral. Logistic regression modeling showed that local anesthesia was more frequently applied in older children (odds ratio=1.041) and for unilateral tympanostomy tube insertion (odds ratio=8.990). The cut-off value of age for local anesthesia was roughly 5 years.
Conclusions
In a pediatric population at a single medical center, age and whether unilateral or bilateral procedures were required were important factors in selecting an anesthesia method for tympanostomy tube insertion. Our findings suggest that local anesthesia can be preferentially considered for children 5 years of age or older, especially in those with unilateral otitis media with effusion.
Tympanostomy tube insertion (TTI), which is usually performed under general anesthesia, continues to be one of the most commonly performed surgical procedures in children worldwide. TTI can be performed under one of endotracheal inhalation, face-mask inhalation, or intravenous anesthesia. Although several studies have demonstrated that above anesthesia methods used for this procedure are relatively safe, with a low incidence of complications [1,2], clinicians should keep in mind the potential risks, including hypoventilation, airway obstruction, seizure, anaphylaxis, and cardiopulmonary arrest. These potential risks are more likely to occur in patients with comorbid medical conditions or a concurrent acute illness such as a respiratory virus [1,2,3]. Despite the low incidence of major complications, their potential seriousness requires that anesthesia and sedation be administered by a team member skilled in airway management, necessitating referral to a secondary or tertiary care setting.
Recently, face-mask inhalation and intravenous anesthesia have increasingly become preferred for TTI in children. However, there are no published guidelines on the choice of anesthesia method, nor is there published evidence to support the use of one method over another. In current practice, the choice to use general anesthesia is often due to the surgeon's belief that local anesthesia provides inadequate pain control for TTI. The use of face-mask inhalation or intravenous anesthesia at secondary and tertiary care centers considerably increases the total medical costs for both the patient and the medical system. One of authors (D.H.L.) has successfully performed many TTI procedures under local anesthesia at an outpatient clinic in the past several years. He typically attempts TTI under local anesthesia first, and if the attempt fails, then the procedure is performed under face-mask inhalation or intravenous anesthesia in an operating room.
This study had two goals. The first was to determine the epidemiologic characteristics of children undergoing TTI under local anesthesia and to compare these data with those of children receiving face-mask inhalation or intravenous anesthesia. Second, we aimed to determine the relationship, if any, between a patient's procedural outcome and the chosen anesthesia method. Ultimately, we aimed to identify criteria that would help physicians make an informed decision on which anesthesia method to use for TTI in children with otitis media. To our knowledge, this study is the first one to evaluate the anesthesia method of pediatric TTI, including financial considerations as well as clinical factors.
We reviewed the medical records of all children who were candidates for TTI at a university-based, secondary referral hospital between 2003 and 2012. Inclusion criteria of TTI group were as follows: 1) diagnosed otitis media with effusion (OME); 2) ears with a retracted or adherent tympanic membrane; and 3) patients for whom TTI was performed by a single surgeon (D.H.L.). Exclusion criteria were as follows: 1) diagnosed acute suppurative otitis media; 2) patients with any abnormality of the external ear or ear canal; and 3) patients for whom TTI was only one of multiple surgeries performed concurrently, including tonsillectomy, adenoidectomy, or frenotomy. Patients in whom several TTIs were performed for a single episode of OME were treated as a single case. Otherwise, each TTI procedure was counted separately.
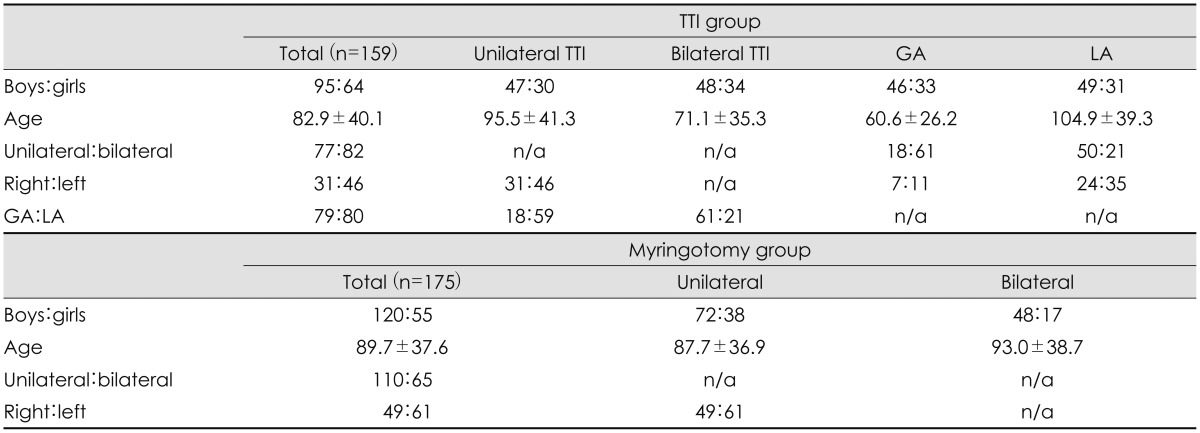
Fig. 1 shows the decision-making flow chart for selecting the procedure and anesthesia method. A total of 159 children (95 boys and 64 girls) were included in the TTI group. Their mean age was 82.9±40.1 months. Unilateral TTI was performed in 77 children (right in 31 and left in 46 children) and bilateral TTI was performed in 82 children. TTI was performed under local anesthesia in 80 children and under intravenous, face-mask inhalation, or endotracheal inhalation anesthesia in 79 children. Of these 79 patients, 12 received intravenous anesthesia using ketamine; 64 received intravenous as well as face-mask inhalation anesthesia; and 3 received endotracheal inhalation anesthesia for TTI.
To establish a control, we reviewed the records of children who received myringotomy alone without TTI under local anesthesia by the same surgeon during the same period. Inclusion criteria of myringotomy alone were as follows: 1) diagnosis of OME; 2) diagnosis of acute suppurative otitis media; 3) ears with a retracted or adherent tympanic membrane; and 4) patients for whom myringotomy was performed under local anesthesia by a single surgeon (D.H.L.).
The myringotomy group included 175 children (120 boys and 55 girls) who met inclusion criteria. Their mean age was 89.7±37.6 months. Unilateral myringotomy was performed in 110 children (right in 49 and left in 61 children) and bilateral myringotomy was performed in 65 children.
Myringotomy or TTI was performed under local anesthesia in an outpatient clinic as follows: patients were placed in a seated position and the ear canal was thoroughly cleaned using microforceps under an operating microscope. The surgeon then inserted small cotton balls into the ear canal adjacent to the tympanic membrane. A 10% xylocaine solution was used to soak the cotton ball completely. After 15-20 minutes, the xylocaine solution was vacuumed out and the cotton ball was removed using microforceps. Myringotomy and/or TTI was performed in the routine manner. For patients with acute suppurative otitis media, myringotomy was performed after a short course of anti-inflammatory drugs and/or oral antibiotics relieved subjective pain and resolved the physical findings of acute inflammation.
Patients who received intravenous and face-mask inhalation anesthesia did not require overnight hospital stay; those who received endotracheal inhalation anesthesia required hospital admission for 2 nights. Cases in which myringotomy alone or TTI was performed under local anesthesia were grouped into the local anesthesia group, while those receiving intravenous, face-mask inhalation, or endotracheal inhalation anesthesia were grouped into the general anesthesia group.
Data collected included the patient's gender, age, diagnosis, procedure performed, types of tubes used, laterality, and type of anesthesia used. Procedure complications were reviewed in the medical chart. Data were analyzed using IBM SPSS software (version 19.0, International Business Machines Corp., Armonk, NY, USA) and R version 2.15.2 (The R Foundation for Statistical Computing). A recursive partitioning procedure and receiver operating characteristic curve analysis were used to determine cut-off values. A p-value less than 0.05 was considered statistically significant.
Epidemiologic data are summarized in Table 1. A Paparella type 1 tube was inserted in 232 ears of 150 children. A Goode T-tube was inserted in 9 ears of 9 children, which included 3 children with a history of cleft palate, 5 children in whom a Paparella type 1 tube was extruded prematurely, and 1 child whose tympanic membrane was particularly thick.
To evaluate the difference according to different surgical techniques, the study group was TTI under local anesthesia and the control group was myringotomy alone under local anesthesia. When comparing the myringotomy and TTI groups, there were no significant differences in gender (p= 0.093; chi-square test), age (p=0.113; independent t-test), or laterality (p=0.560; chi-square test). However, unilateral procedures were performed more frequently in the myringotomy group than in the TTI group (p=0.008; chi-square test).
In the myringotomy group, there was no significant difference in gender (p=0.248; chi-square test) or age (p=0.368; independent t-test) between patients receiving unilateral and bilateral procedures. In the TTI group, there was no significant difference in gender between patients receiving unilateral or bilateral procedures (p=0.748; chi-square test) but age was significantly higher in cases requiring only a unilateral procedure (p<0.0001; independent t-test).
To evaluate the difference according to different anesthesia methods, the study group was TTI under local anesthesia and the control group was TTI under general anesthesia. When comparing the local and general anesthesia groups, there was no significant difference in gender (p=0.698; chi-square test) or laterality (p=0.892; chi-square test) but age was significantly higher in the local anesthesia group than in the general anesthesia group (p<0.0001; independent t-test). Unilateral TTI was performed more frequently under local anesthesia, but bilateral TTI was performed more frequently under face-mask inhalation or intravenous anesthesia (p<0.0001; chi-square test).
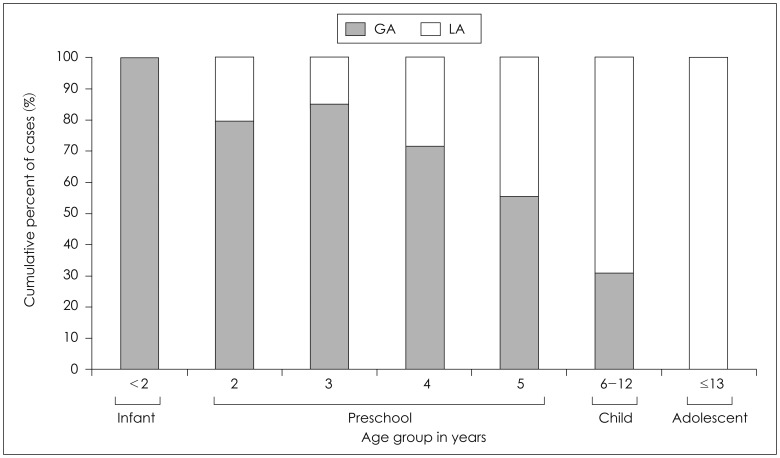
Fig. 2 shows that many preschool-aged children received face-mask inhalation or intravenous anesthesia for TTI, while local anesthesia was sufficient for older children. Logistic regression analysis showed that administration of local anesthesia increased with age (odds ratio=1.041, p<0.0001), and local anesthesia was more frequently used in cases of unilateral TTI (odds ratio=8.990, p<0.0001). The cut-off value for age in the use of local anesthesia was 67 months. In other words, children older than 5 years were more likely to undergo TTI under local anesthesia.
In this study, 8 children (7 boys and 1 girl; mean age= 63.4±37.7 months) did not undergo TTI under local anesthesia, even though myringotomy was done under local anesthesia. Four children may have been too young to undergo the procedure (mean age=39.3±10.9 months); and 4 children had a severely adhesive tympanic membrane (Sade's stage 3 or 4) that caused intolerable pain during tube insertion.
Multiple TTIs were performed in 28 children (17 boys and 11 girls; mean age=91.2±42.4 months-old) with a mean TTI frequency of 2.6±1.2 (range, 2-7). Of the 74 TTI procedures performed in these 28 children, 41 were indicated by longstanding OME and 33 were required for OME complicated by a retracted or adhesive tympanic membrane. Among these 28 children, 9 had their first TTI under general anesthesia and their second procedure under local. The mean age difference between procedures in these 9 children was 9.0±4.8 months (range, 2.0-17.0).
This study found that local anesthesia can be successfully used for TTI in older children, particularly those aged 5 years and older, while face-mask inhalation or intravenous anesthesia was more commonly used in preschool-aged children. In clinical practice, however, it is currently standard to perform TTI under intravenous anesthesia using ketamine, facemask inhalation anesthesia, or both [4], despite potentially dangerous side effects. For example, children requiring TTI often have an upper respiratory tract infection, which increases the risk of laryngospasm with inhalational anesthesia [2,5]. In addition, the use of ketamine in children can prolong the recovery period and result in emergence delirium, dizziness, nausea, vomiting, and increased oral secretions [6]. Given these side effects, most pediatric anesthesiologists add other sedatives or analgesics to improve the quality of procedural sedation and analgesia [6,7]. Other pediatric procedures that traditionally require general anesthesia include tympanostomy tube removal, patch myringoplasty, foreign body removal from the ear or nose, fine-needle aspiration biopsy, and simple frenotomy.
This study showed that unilateral procedures were performed more frequently in patients requiring myringotomy alone, while bilateral procedures were more frequent in the TTI group. This is likely a result of clinical practice guidelines for otitis media in children, which recommend that TTI be performed in bilateral OME.
Most of the children in this study who underwent myringotomy or TTI under local anesthesia did not feel any pain during the myringotomy or tube insertion. A considerable portion of children who underwent TTI under local anesthesia complained of a sensation of fullness sensation or vague discomfort while the tube was inserted. This may be explained by the fact that the tympanostomy tube presses on the tympanic membrane, resulting in excessive medialization of the stapes into the cochlea. Many children experienced a loud noise while the effusion was suctioned out, and younger children sometimes were startled and cried. However, this did not interrupt the completion of TTI under local anesthesia. Only a few children complained of intolerable pain during the TTI procedure. These children felt pain when the tube contacted the middle ear mucosa, which may have been due to in adequate anesthesia of the middle ear mucosa.
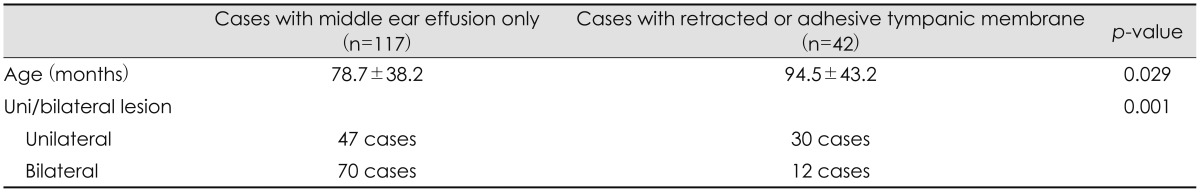
This study found that age was significantly older when a unilateral procedure was indicated. Younger children may tend to need bilateral TTI due to immaturity of their eustachian tubes and resulting symmetric dysfunction. Although anatomic changes in the eustachian tubes during growth and development tend to increase the efficiency of tubal opening, asymmetric growth and development may lead to dysfunction in some children [8]. Our findings support the hypothesis that the indications for TTI in older children may differ from those in younger children. We also found that patients with a retracted or adhesive tympanic membrane (mean age=94.5± 43.2 months) were significantly older than those with middle ear effusion only (mean age=78.7±38.2 months; p=0.029, independent t-test). In comparison to patients with a retracted or adhesive tympanic membrane, those with middle ear effusion underwent bilateral TTI more frequently (p=0.001; chi-square test) (Table 2).
In this study, unilateral TTI was performed more frequently under local anesthesia and bilateral TTI was performed more frequently under general. As discussed above, this finding may be due to the fact that younger children require bilateral TTI due to symmetric dysfunction of immature eustachian tubes, but not due to shorter operation time of unilateral TTI than bilateral. In this study, no patients underwent a bilateral procedure in which TTI under local anesthesia succeeded on one side but failed on the other. Based on finding, we can hypothesize that the TTI procedure itself did not influence the choice of anesthesia method.
Proper selection of anesthesia method can significantly reduce medical costs. In a United States patient population under 18 years of age, Shiley, et al. [3] compared the efficacy, safety, and cost of common pediatric otolaryngology procedures using intravenous anesthesia in the outpatient clinic versus general anesthesia in the operating room. They found that average hospital charges were significantly higher for general anesthesia (USD 356.22 in the intravenous anesthesia group vs. USD 1516.55 in the general anesthesia group). They explained that the surgeon's fees and hospital charges were separated and that the former was based on current procedural termin ology code and not affected by hospital location, but that the latter depended on where the procedure was performed. Hospital charges were higher in the operating room, and anesthesia charges increased in proportion to procedure time. In contrast, the National Health Insurance System of South Korea does not separate the physician's fee from hospital charges. Anesthesia fees are added when the procedure is performed under intravenous or general anesthesia, and additional hospital charges apply for overnight admission. In South Korea, the minimum hospital charges for unilateral TTI performed by a pediatric otolaryngologist at a secondary or tertiary referral hospital are USD 200-220 if done under local anesthesia and USD 400-420 if done under intravenous or face-mask inhalation anesthesia. The minimum hospital charge increases to USD 520-550 for a single night of hospital observation after endotracheal inhalation anesthesia. In the case of general anesthesia (intravenous, face-mask inhalation, or endotracheal inhalation), an additional charge of USD 80-85 is assessed for preoperative medical workup, including electrocardiogram, chest X-ray, and routine blood tests. Therefore, when outpatient TTI is performed under local anesthesia, the burden of total medical costs can be decreased 2- to 3-fold, and patient charges can be decreased 1.5- to 2- fold.
This study has several limitations, including its retrospective design, although we strictly defined inclusion and exclusion criteria. In addition, the potential impact of our findings on medical costs depends on the country in question. This study enrolled only cases in whom TTI was performed by a single surgeon, which could make some possible bias unintentionally. The major limitation of this study was that we could not survey patients' response to anesthesia and TTI. Because of its retrospective design, this study could review only side effect like seizures, anaphylaxia and cardiopulmonary arrest. Younger patients can feel that even brief surgery is agitated under local anesthesia that under general. However, their parents may feel against agitation, nausea, vomiting or prolonged recovery of general anesthesia.
This study found that local anesthesia group was significantly older than in general anesthesia group. Based on our experience, it is very important to choose which children can get TTI under local anesthesia and to build up a trusting relationship with children before surgery. They are a vulnerable client group as they differ emotionally, psychologically, and physiologically from adults. In order to minimize anxiety and optimize the surgery, watchful waiting for 3 months is enough to figure out child's tendency and to build up a trusting relationship with child and parents before surgery. In our study, all children who underwent their first TTI with local anesthesia also underwent their second TTI under local anesthesia. This may be due to the significant length of time that elapsed between procedures; for example, the youngest child who underwent TTI under local anesthesia 40.2 months old at the first procedure and 53.6 months old at the second.
The 10% xylocaine solution as well as EMLA can make enough anesthetic effect to do TTI. The penetration of these drugs through the skin involves diffusion via transcellular and intercellular pathways, and via hair follicles and sweat glands. These anesthetic drugs inhibit the initiation and propagation of nerve firing in the sensory nerves distributed in the ear canal and tympanic membrane [9]. Without a vehicle which maximizes drug delivery into the skin or a penetration enhancer which enters into the skin and alters it reversibly to promote the drug absorption, 10% xylocaine solution-soaked cotton ball can give enough anesthetic effect to do TTI in children. It is very important to keep 10% xylocaine solution-soaked cotton ball in touch with tympanic membrane. The advantage of 10% xylocaine solution than EMLA is easy to clean up the ear canal.
The surgery under local anesthesia has some benefits; it does not need laboratory evaluation, such as chest X-ray; the surgery can be performed even for mildly sick child, such as common cold; it can shorten the hospital stay; it can avoid potential risk of general anesthesia; it can shorten the recovery time and enhance the safety; and it can give the costal saving.
This study demonstrates that pediatric TTI can be successfully performed under local anesthesia. Two factors significantly related to anesthesia method were the patient's age and whether a unilateral or bilateral procedure was required. Based on our findings, we suggest that local anesthesia can be preferentially considered in children 5 years and older, especially for unilateral TTI. Based on our cost analysis, we believe that a rational anesthesia choice can significantly decrease the health care costs associated with TTI. To our knowledge, this study is the first one to evaluate clinical factors of pediatric TTI, together with financial considerations in Korea.
References
1. Hoffmann KK, Thompson GK, Burke BL, Derkay CS. Anesthetic complications of tympanostomy tube placement in children. Arch Otolaryngol Head Neck Surg 2002;128:1040–1043. PMID: 12220208.


2. Markowitz-Spence L, Brodsky L, Syed N, Stanievich J, Volk M. Anesthetic complications of tympanotomy tube placement in children. Arch Otolaryngol Head Neck Surg 1990;116:809–812. PMID: 2363918.


3. Shiley SG, Lalwani K, Milczuk HA. Intravenous sedation vs general anesthesia for pediatric otolaryngology procedures. Arch Otolaryngol Head Neck Surg 2003;129:637–641. PMID: 12810468.


4. Lee JA, Jeon YS, Noh HI, Choi JW, In JH, Kim YM, et al. The effect of ketamine with remifentanil for improving the quality of anaesthesia and recovery in paediatric patients undergoing middle-ear ventilation tube insertion. J Int Med Res 2011;39:2239–2246. PMID: 22289539.


5. Green SM, Roback MG, Kennedy RM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med 2011;57:449–461. PMID: 21256625.


6. Gloor A, Dillier C, Gerber A. Ketamine for short ambulatory procedures in children: an audit. Paediatr Anaesth 2001;11:533–539. PMID: 11696116.


7. Novak H, Karlsland Akeson P, Akeson J. Sedation with ketamine and low-dose midazolam for short-term procedures requiring pharyngeal manipulation in young children. Paediatr Anaesth 2008;18:48–54. PMID: 18095966.


8. O'Reilly RC, Sando I. Anatomy and physiology of the eustachian tube. In: Flint PW, Haughey BH, Niparko JK, Richardson MA, Lund VJ, Robbins KT, . editors. Cummings Otolaryngology: Head & Neck Surgery. 5th ed. Philadelphia: Elsevier Mosby;2010. p.1866–1875.
9. Tadicherla S, Berman B. Percutaneous dermal drug delivery for local pain control. Ther Clin Risk Manag 2006;2:99–113. PMID: 18360585.


Fig. 1
Flow chart of the selection process for procedure and anesthesia method. TTI: tympanostomy tube insertion, GA: general anesthesia including face-mask inhalation or intravenous anesthesia, LA: local anesthesia.
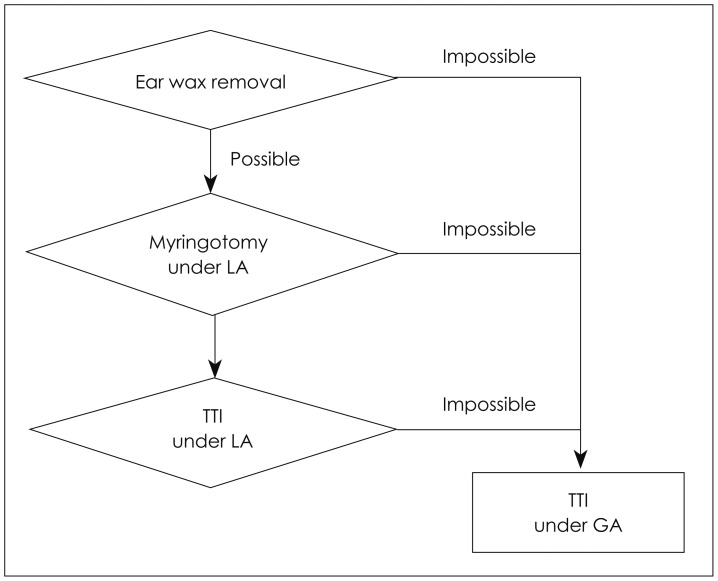
Fig. 2
Distribution of anesthesia methods according to age. The x-axis represents age groups in years and the y-axis represents the cumulative percent of cases. GA: general anesthesia including face-mask inhalation or intravenous anesthesia, LA: local anesthesia.