Effect of Tianeptine on Depressed Tinnitus Patients
Article information
Abstract
Background and Objectives
Tianeptine is a tricyclic antidepressant that has a novel pharmacological property: it increases the reuptake of 5-hydroxytryptamine. Recent studies have reported that the prevalence of depression is greater in patients with tinnitus than in control subjects who do not have tinnitus. The purpose of this study was to assess the efficacy of tianeptine for the relief of tinnitus, especially in patients with depressive mood.
Subjects and Methods
Among a total of 52 tinnitus patients, 15 had depressive mood. The depressed tinnitus patients were prescribed Stablon® 12.5 mg once daily for 1 month without any other drug. We assessed the severity of tinnitus, level of depression, and the quality of sleep in these patients by using the Tinnitus Handicap Inventory (THI), Beck Depression Inventory (BDI), and Pittsburgh Sleep Quality Index (PSQI). Hearing impairment and severity of tinnitus were measured with pure tone audiometry, speech audiometry, and tinnitograms. These evaluations were conducted before and after medication treatment.
Results
For the 15 depressed tinnitus patients, THI scores significantly correlated with BDI and PSQI scores prior to medication treatment. These results showed that the discomfort of tinnitus was closely related to depression and sleep disorder. After medication treatment, THI and BDI scores significantly decreased, indicating that tinnitus and depression improved. However, no significant alteration in PSQI score was observed, indicating that there was no improvement in sleep quality.
Conclusions
In the treatment of depressed tinnitus patients, tianeptine might be an efficient drug to treat both tinnitus and depression. However, tianeptine is unlikely to improve the quality of sleep in these patients.
Introduction
Tianeptine is not a typical antidepressant drug; chemically, it is a tricyclic antidepressant (TCA); however, it possesses the pharmacological property of increasing 5-hydroxytryptamine uptake. As a result of this mechanism, tianeptine has a faster onset of antidepressant effect, better efficacy among selective serotonin reuptake inhibitors (SSRIs) [1], and fewer adverse effects than typical tricyclic antidepressants and SSRIs do [2]. Several pre-clinical studies have revealed that tianeptine also has a beneficial effect on depression and various stress-induced disorders [34].
Tinnitus is the phantom perception of sound that results from activity within the nervous system without any corresponding mechanical or vibratory activity within the cochlea, and is not related to any external stimuli [5]. It is estimated that one-third of the global population experiences tinnitus at least once in their lifetime, and about 1-5% of these affected individuals experience serious psychosocial complications [6]. Recent studies have reported that tinnitus patients are likely to have comorbid psychological disorders including depression and anxiety [78], and show a high prevalence of depression [910]. In addition, the severity of tinnitus has been positively correlated with levels of depression [111213].
There is no definite cure for tinnitus. Management of tinnitus requires a multi-disciplinary approach depending on the cause and comorbid conditions of tinnitus patients. Currently, there are no FDA-approved drugs to treat tinnitus, however, clinical studies are underway to evaluate the efficacy of N-methyl-d-aspartate and dopamine D2 antagonists, SSRIs, and γ-aminobutyric acid (GABA) agonists [14]. Previous studies suggest that patients with severe depression may experience improvement in their tinnitus after treatment with antidepressants such as nortriptyline [15] or sertraline [16].
In this study, we investigated the relationship among the severity of tinnitus, the level of depression, and the quality of sleep in depressed tinnitus patients. We also evaluated the efficacy of tianeptine on treating tinnitus with depressive mood.
Subjects and Methods
Patients
A total of 52 patients who visited the otorhinolaryngology outpatient clinic of tertiary hospital from 2009 through 2014 and were first diagnosed as having tinnitus with were prospectively investigated. All patients underwent history interviews, physical examinations, hearing tests, and answered questionnaires. Questionnaires on tinnitus, depression symptoms, and quality of sleep were completed at the first visit. Patients with acute tinnitus (<3 month), otologic disease, history of previous treatment for tinnitus or systemic disease (Hypertension, diabetic mellitus or cardiovascular disease) were excluded.
The patient provided written informed consent to participate in this study, which was approved by the local Institutional Review Board for Research (ED15142-3).
Evaluation of depression symptoms and study design
The Korean version of the Beck Depression Inventory (BDI) was used to evaluate the severity of depression symptoms in patients. It comprises 21 questions, which includes the emotional, cognitive, motive, and physiological areas of depression. Each question is rated on a scale from 0 to 3, depending on the degree of symptom, and the total score is calculated from a range of 0 to 63. A previous study found that a BDI score of 16 or above for men, and 17 or above for women is classified as depression [17]. Based on these criteria, tinnitus patients were divided into two groups: the control group and the depressed group.
Medication
History taking, physical examinations, questionnaires, and hearing tests were performed in 52 tinnitus patients. Of these, only 15 patients had depressive mood according to the Korean-version BDI. These depressed tinnitus patients were administered tianeptine (Stablon®, JEIL, Seoul, Korea) 12.5 mg once daily for 1 month with no other medications. Patients revisited out-patient clinic with 2 weeks, 4 weeks. Evaluations for tinnitus, depression, and quality of sleep were conducted before and after medication use.
Evaluation of tinnitus
To evaluate the severity of tinnitus, the Tinnitus Handicap Inventory (THI) was administered to patients. The Korean-version THI measures the impact of tinnitus on daily life and its reliability and validity were proven through a previous study [18]. It contains 25 items with a functional subscale (11 items), emotional subscale (9 items), and catastrophic subscale (5 items). Each question is rated as 0 (none), 2 (sometimes), or 4 (always). The total score is calculated from a range of 0 to 100.
Evaluation of sleep quality
The Korean version of the Pittsburgh Sleep Quality Index (PSQI) was used to assess the quality of sleep [19]. It comprises 19 items, which measure subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime function. Each question is rated from a scale of 0 to 3 depending on the degree of symptoms, and the total score is calculated from a range of 0 to 21. A total score of 5 or above indicates poor sleep quality.
Hearing test
Pure tone audiometry, speech audiometry, and tinnitograms were performed to check for hearing and tinnitus status of patients.
Statistical analysis
Statistical analysis was performed using the SPSS 21.0 (SPSS Inc., Chicago, IL, USA) program. The Pearson bivariate correlation test was used to analyze correlations between variables. Qualitative variables were analyzed using Fisher's exact test to compare differences between groups. A paired sample t-test was used to compare changes in THI, BDI, and PSQI scores before and after the medication use. All data were expressed as means±standard deviation. The level of statistical significance was set as p<0.05.
Results
Characteristics of depressed tinnitus patients
A total of 52 tinnitus patients were diagnosed as having tinnitus. According to the BDI score criteria, tinnitus patients were stratified into two groups according to the presence of depressive mood. Thirty-seven (71.2%) patients without depressive mood were in the control tinnitus group and 15 (28.8%) patients with depressive mood were in the depressed tinnitus group. As shown in Table 1, more female patients were observed in the depressed tinnitus group, which was statistically significant (p=0.031). The mean THI score of the depressed tinnitus group was 51.67 (±19.58), which was significantly higher than that in the control tinnitus group (p=0.005). No significant differences in the severity of tinnitus, age, pure tone audiometry and PSQI score were found.
Correlation among THI, BDI, PSQI in depressed tinnitus patients
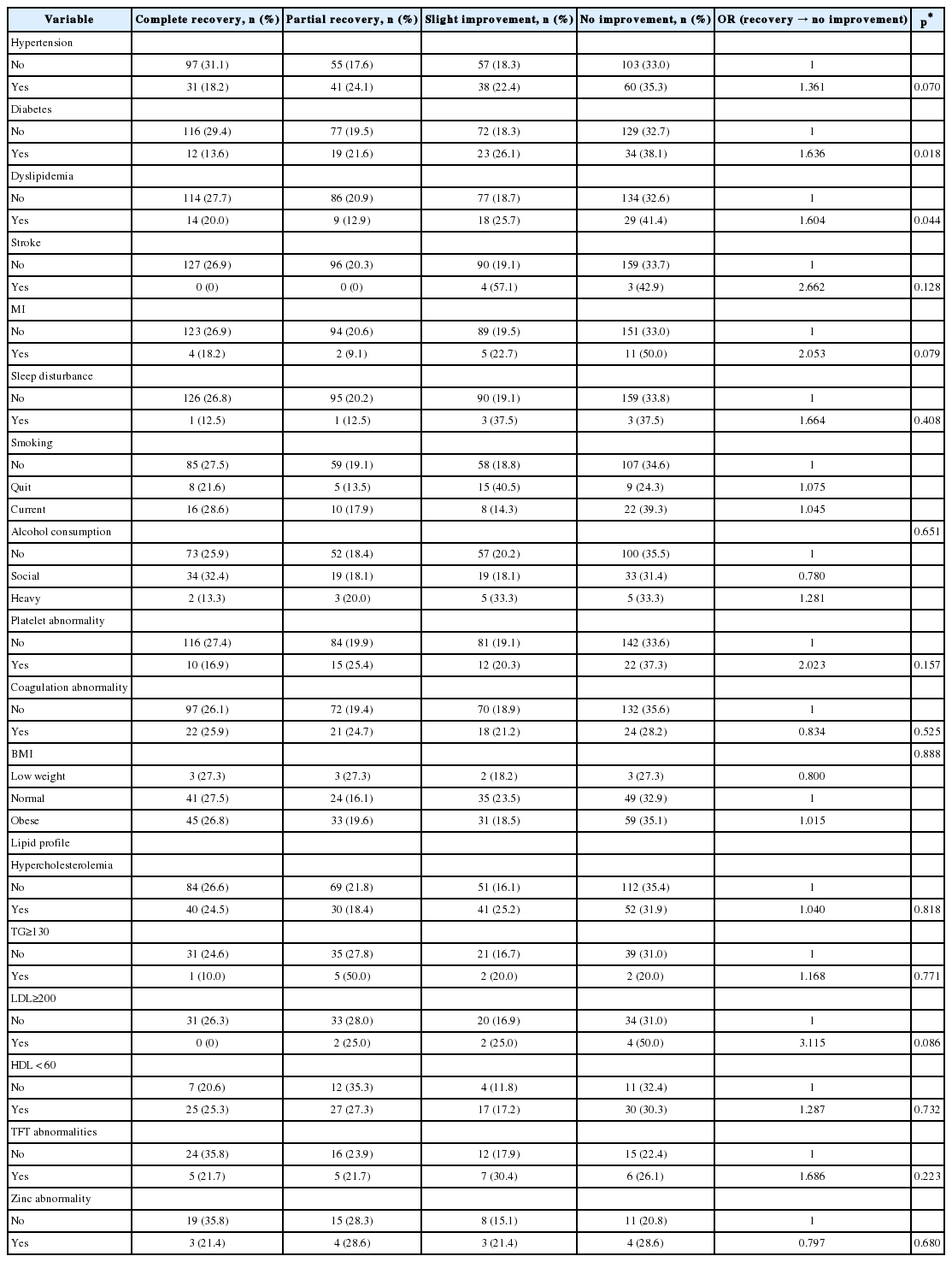
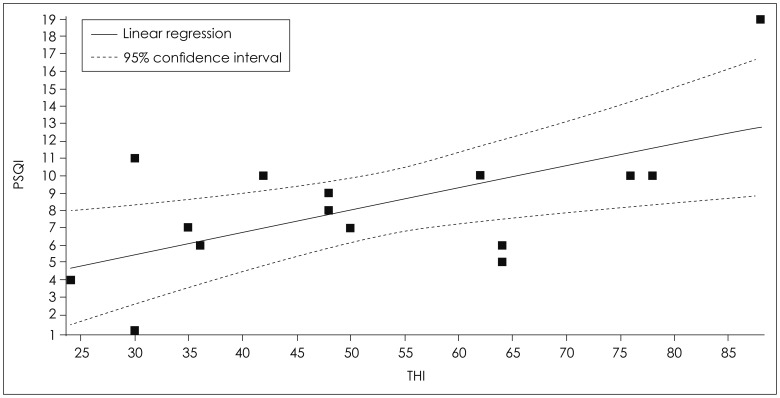
Next, we investigated the relationship among THI, BDI, PSQI scores in depressed tinnitus patients. Table 2 shows correlations of depressed tinnitus patients based on THI and BDI scores, THI and PSQI scores, and BDI and PSQI scores, respectively. There was a significant correlation between THI and BDI scores (r=0.5758, p=0.0247) (Fig. 1) and between THI and PSQI scores (r=0.6151, p=0.0147) (Fig. 2). However, there was no significant correlation between BDI and PSQI scores in depressed tinnitus patients (Table 2).

Correlation between THI and BDI in depressed tinnitus patients. There was a significant correlation between THI and BDI scores (r=0.5758, p=0.0247). THI: Tinnitus Handicap Inventory, BDI: Beck Depression Inventory.
Effects of tianeptine on THI, BDI, and PSQI scores in depressed tinnitus patients
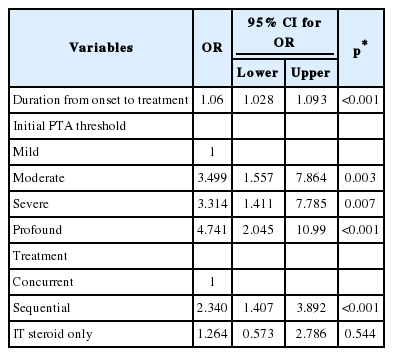
To evaluate the efficacy of tianeptine on tinnitus, depression symptoms, and the quality of sleep, 15 depressed tinnitus patients were administered tianeptine (Stablon®) 12.5 mg once daily at bedtime for 1 month and were evaluated for the severity of tinnitus, THI, BDI, and PSQI scores before and after medication treatment. After medication treatment, the mean score of THI improved from 51.67 (±19.58) to 43.07 (±18.68) and those of BDI improved from 24.71 (±6.13) to 15.53 (±4.10), which were statistically significant (p=0.0031, p<0.001, respectively). Tianeptine had no significant improvement on the PSQI score (Table 3). Furthermore, Table 4, 5 show the improved score of each item of THI and BDI, respectively, with tianeptine treatment. The functional subscale and emotional scale of THI score was significantly improved with tianeptine treatment (p=0.020, p=0.012) (Table 4). Interestingly, the mean PSQI score was not significantly altered after tianeptine treatment but an item of sleep latency significantly improved (p=0.023) (Table 6).
Discussion
There is a 5% prevalence of major depression in the public and it is reported that the probability of depression occurring at least once in a lifetime is 20% in women, and 10-15% in men [20]. Tinnitus is a common symptom with 10-15% prevalence in the general population, and it negatively affects 1-2% of these individuals during normal activities. According to previous reports, approximately 39% of tinnitus patients also have major depression [21]. In our study, 15 (28.8%) of 52 tinnitus patients showed a propensity for depressive mood compared to control patients. The reason for the higher percentage of depressive mood in women who have tinnitus is that they have greater predisposition to depression than men, which has a high impact according to the prevalence of depression. However, there was a higher proportion of women with tinnitus who visited the hospital for treatment. Furthermore, according to the threshold of predisposition to depression, which was 17 points in women and 16 points in men from The Study on Standardization of BDI, women usually have more depression symptoms than men.
The aims of this study were to prove the correlation between tinnitus and depression and to investigate a beneficial effect of treating tinnitus patients with depressive mood. Particularly, in depressed tinnitus patients, THI scores were positively correlated with PSQI and BDI scores with statistical significance. These results show that the discomfort of tinnitus, depression, and sleep disorders were closely related. Next, tianeptine significantly improved tinnitus (total THI score), depression (total BDI score), and sleep latency in depressed tinnitus patients. However, there was no statistically significant improvement in the quality of sleep (total PSQI score). Based on the results of this study, tianeptine might be an efficient mediation to treat both tinnitus and depression symptoms in tinnitus patients with depressive mood. We could consider the order-relationship of depression and tinnitus in depressed tinnitus patients. Dobie, et al. [22] reported that more than 50 percent of tinnitus patients already had major depressive disorder before the occurrence of tinnitus. Only 7% of depressed patients had tinnitus before being diagnosed for depression [23]. In other words, patients with depression are more likely to experience tinnitus. When reviewing other reports, tinnitus is not an independent factor to trigger depression, but it can be an important factor in patients with sensitivity to mental illness. There is no proof that depression can directly cause tinnitus. There was no significant difference between patients with depression and those without [20]. However, people with depression sometimes have an inadequate physical response, therefore, the tinnitus, which was previously ignored, may feel worse [24]. The key factor in explaining why some tinnitus patients feel a little discomfort while others are distressed is the psychological aspect associated with depression. As such, since depression has a higher associated morbidity and a close relationship with tinnitus, it is possible to administer antidepressants for the treatment of tinnitus [21].
In the past, a number of studies reported on tinnitus treatment with TCAs [202225]. Recent studies focus on SSRIs, which have less adverse effects than TCAs. In a study of severe tinnitus accompanied with depression, administration of sertraline showed meaningful improvement of tinnitus compared to placebo [21]. After tinnitus with depression was treated with different types of SSRIs, improvement of tinnitus was reported [26]. The mechanism of the effects of antidepressants on tinnitus has not yet been established. The main hypothesis is that antidepressants may not directly affect tinnitus, but the depression accompanied with tinnitus. This is supported by the fact that in patients with severe depression, their subjective tinnitus improved with treatment with nortriptyline [1527]. Furthermore, patients with depression may be more sensitive to internal or external noise than those without depression [22]. Another hypothesis is that SSRIs can reduce tinnitus symptoms directly by interfering with the transmission of tinnitus impulses [28]. This is supported by a number of documents that there are a large number of serotonin receptors in the auditory nervous system and variation of these receptors can generate auditory evoked potential [2930]. In some reports, antidepressants, including TCAs and SSRIs, can cause tinnitus as a side effect in some patients [16], but the tinnitus was reversible when the drugs were stopped. Tinnitus treatment with antidepressants, as current studies have shown, is considered to be the most effective to use in tinnitus patients with depression.
This paper is a prospective study that observed an improvement in tinnitus by treatment with tianeptine alone in tinnitus patients with depressive mood. We look forward to a choice of new drugs for the treatment of tinnitus in the ENT area. Tianeptine is a good treatment of choice in severe tinnitus patients with depressive mood, but they cannot control sleep disorders. Therefore, it can be helpful to co-administer with sedatives or hypnotics that are not addictive.
In this study, there was no control group using other antidepressants or placebo. We need clinical studies examining a larger number of patients for a long period and comparing medications including other antidepressants, blood circulation enhancers or tranquilizers to investigate relative efficacy of tianeptine.
In conclusion, tianeptine is good alternative treatment in depressed tinnitus patients because it is an effective agent to reduce both symptoms. In this case, additional treatments are required to control sleep disorders.
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (NRF-2014-071497; R1429733); Korea University research grant (K1609821); and Korea Health Industry Development Institute (R1606511). These funding sources only provided financial support and played no specific scientific role in this study.
Notes
Conflicts of interest: The authors have no financial conflicts of interest.