 |
 |
- Search
| J Audiol Otol > Volume 24(1); 2020 > Article |
|
Abstract
Because the psychophysical symptoms of hearing loss and dementia in the elderly are very similar, untrained healthcare professionals in dementia facilities can easily overlook a severity of hearing loss in their patients. The present study identifies their knowledge, attitudes, and practices (KAP) on hearing loss using a survey whether they may help hearing problem of the patients with dementia. A total of 29 health-care professionals responded to the KAP survey. Also, 2 family members participated. The results showed that most of the nurses and caregivers in elderly medical welfare facilities who worked with dementia patients did not have knowledge of their hearing loss. Even the facility managers did not know how to conduct hearing tests for their patients although they did recognize that some of their patients had a hearing loss. Eventually, actual practice was not possible at this moment by the professionals. However, our respondents did have a positive attitude toward screening for hearing loss and help their patients with dementia wear hearing aids if a clinical guideline was provided. We suggest to develop clear and precise clinical guidelines of the hearing screening test for the dementia patients due to the interrelationship between dementia and hearing loss. When these guidelines apply to elderly residents in a medical welfare facility, early diagnosis and treatment of their sensory loss will help alleviate their dementia as well.
Since improved surgical procedures and treatment techniques have made it possible to overcome various maladies, the human life span has been extended; thus, the number of older adults is increasing globally. South Korea is also showing the same unprecedented rapid aging trend. According to the report by Korean Statistical Information Service, its ratio of elderly population will reach 20% of total population in 2025, making Korea a super-aged society [1]. Thus, common chronic diseases of the elderly are currently considered carefully at the government level, along with a need for better care of the elderly.
The elderly with dementia is globally estimated at 35.6 million as of 2012 and forecast to triple by 2050 [2]. Given that new attention, there is strong evidence that the degraded functioning of aging sensory systems may be associated with cognitive decline in the elderly. Contemporary researchers have thus investigated the relationship between hearing and/or vision impairments of old adults and cognitive dysfunction. As examples, we summarize here eight well-designed studies [3-10] in Table 1. Although the methodology applying for functional and dysfunctional measurements of the sensory and cognitive systems were slightly different across these studies [3-5,9], all concluded that either hearing or vision loss in the older population could fatally affect any dementia. In particular, the symptoms caused by untreated hearing loss showed very similar tendencies for worsening cognitive decline or dementia, while limiting social activity and producing isolation, depression, a lower quality of life, and reduced mental well-being overall [11,12].
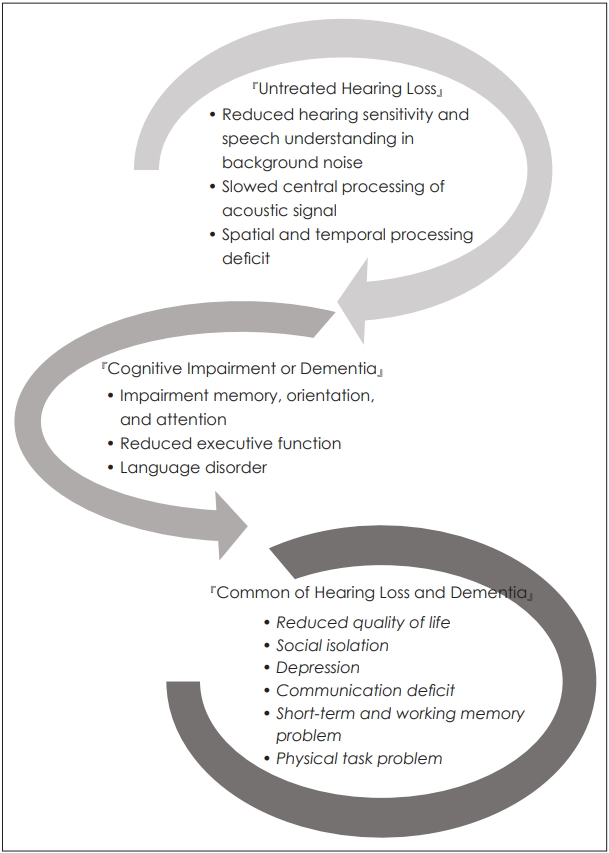
Although each case of hearing loss and cognitive impairment can have a different characteristic due to the different sites of the lesion, i.e., the ear and brain, respectively, Fig. 1 demonstrates that the two diseases share many common psychophysical symptoms, including a lower quality of life, communication disability, social isolation, depression, and more. In other words, any patient who suffers from both dementia and hearing loss, the symptoms of hearing loss may be confusable or covered up as part of the cognitive impairment, thereby resulting in their hearing system remaining untreated. When considering the increased risks for dementia and the significant negative impact of comorbidity of two diseases on the mental well-being of the elderly, it becomes even more necessary to clinically evaluate the hearing loss in dementia patients.
On the other hand, the Knowledge, Attitudes, and Practices (KAP) survey is a representative tool used for a specific population to collect information on what is known, believed, and done in relation to a specific field. Historically, the KAP model was developed for family planning and population studies in the 1950s, with its purpose being to measure the extent to which any clear opposition to the notion and organization of family planning existed among different populations, so specific family planning practices could be used for different program purposes worldwide. In the 1960s and 1970s, the number of studies on community perspectives and human behavior grew rapidly in response to the needs of the primary health care approach that was adopted by international aid organizations [13]. Since that time, these KAP surveys had been used to investigate health behavior and continued to be widely used to gain information on health-seeking practices. Based on the KAP model, knowledge affects attitude and practice directly, and attitude will also directly affect actual practice or intentions [14]. In other words, three factors were related and thus considered together.
This brief communication identifies KAP on hearing loss of the health-care professionals in the elderly medical welfare facilities, while using a questionnaire based on that KAP model. Also, as an early stage of approach, we discuss what can be provide for them and their patients by hearing professionals in Korea
To develop the Korean version of KAP (K-KAP) survey, a questionnaire was adapted [15] with both translation and back-translation from English to Korean by a professional translator, and inappropriate questions related to the Korean health system were modified (i.e., the residential aged care setting in the original version of the KAP survey was modified to be an elderly medical welfare facility and long-term hospitalized facility). The final version of the questionnaire was consulted on and confirmed by professors with long careers in the Audiology and Nursing fields.
The K-KAP survey consisted of four target populations for each version: 1) Facility Manager (46 questions), 2) Nurses and Allied Health Professionals (25 questions), 3) Caregivers (25 questions), and 4) Family Members of Patients (19 questions). The version for facility workers (1 to 3) investigated three aspects of knowledge, attitudes, and practices- related sensory impairments for dementia, while the version of family members included several questions about sensory loss of their patients at the facility. Each version of the questionnaire had the same purpose, but it was slightly different in terms of its scope of gathered information. For example, the version for the facility manager included questions on whether employees were educated for related sensory impairment for patients with dementia, how to reflect support of the management plan, and more. The version for the nurses and allied health professionals and caregivers included questions on whether they had received education about sensory loss and the interpretation of results of screening tests. In other words, the questionnaire was systematically structured in terms of each participantŌĆÖs position and related circumstances.
Before extending in a larger scale study in Korea, participants were randomly contacted to two facilities, one for Namyangju city and the other for Chuncheon city in easy accessibility and short duration of the pilot study. The target participants consisted of four groupsŌĆÖ working at legally designated ŌĆśelderly medical welfare facilitiesŌĆÖ and a ŌĆślong-term hospitalized facility (in Korea, the elderly medical welfare facility provides nursing and assisting other daily life for the elderly, whereas the long-term hospitalized facility has a similar service except for professional medical services to patients by doctors and nurses)ŌĆÖ in Korea and these facility patientsŌĆÖ family member.
For the sample data, a total of 31 subjects completed a questionnaire with a sufficient explanation of its purpose and method. The respondents consisted of 4 facility managers, 5 nurses and allied health professionals, 20 caregivers, and 2 family members of patients. Detailed information on the respondents is included in Table 2.
All procedures for the present study were approved by Hallym UniversityŌĆÖs Institutional Review Broad (HIRB-2018-065) and the participants were asked to sign an informed consent before they completed the questionnaire.
Five facility managers who have worked for nearly two years responded and recognized that a number of the dementia patients with sensory loss and the degree of their loss (4 out of 5). However, none responded and indicated they know how to screen for difficulty of hearing or vision for their patients. In terms of attitude, three out of five managers were able to test the hearing or vision when provided with specific clinical guidelines (or a program manual) and screen their patientsŌĆÖ sensory systems. Although most of the managers did not know the guidelines well, they were positive about monitoring the hearing or vision conditions of their patients and recognized it was as necessity. Nevertheless, current situation indicated that there was no facility or staff training on doing hearing and/or vision tests as a typical practice.
Table 3 displays the responses from 4 nurse and allied health care professionals and 20 caregivers on their knowledge. Although 3 out of 4 nurses partially knew their patients had hearing or vision loss and the way to use to refer them to professionals, they could not conduct simple testing (100%) and also not interpret the results (75%) due to a lack of training and/or knowledge. Thus, they also reported having less confidence in handling assistive devices for hearing and vision. Compared to the responses of the nurses, the answers of caregivers were less knowledgeable and seemed negative.
Regarding attitudes on the KAP survey (Table 4), the respondents partially agreed with conducting screen tests for hearing or vision. In particular, the caregivers wanted more guidance about the clinical guidelines. Also 80% of the caregivers reported that their patients with dementia might actually use hearing aids effectively. In Table 5, our respondents report that most did not test or check the assistive devices of hearing and vision, such as hearing aids and spectacles, while also having no opportunity to be educated or training. There was no specialized staff to care the hearing or vision loss for their patients.
The present study surveyed KAP of staffs in the aged care facility and of family members of residents towards hearing and identified any feasibility of K-KAP survey to find any relation of three factors. The current pilot data showed that most respondents who were nurses and caregivers in the elderly medical welfare facility and had worked for dementia patients did not have any/enough knowledge of the hearing loss of the elderly. Even the facility managers did not know about how to conduct hearing tests for their patients although they did realize that some of their patients had hearing loss. Thus, the practice, e.g., test and interpretation of those results and checking an assistive device, was not possible in the current situation. However, our respondents did some positive attitudes toward screen for hearing loss and helping elderly with dementia wear their hearing aids if specific clinical guidelines were provided.
Although we consider that direct support of hearing and vision impairments, by fitting hearing aids and eye glasses, is unlikely to succeed in the context of more serious cognitive deficits, such as dementia, and many do think about the complexity of concurrent deficits as well as the low rate of access to vision and hearing services in many elderly people, the related studies have proven that untreated hearing loss negatively affects dementia. Although the current data was only a small sample and limited to a specific regional area, there is a lack of systematic care for dementia patients with hearing loss in Korea, which warrants a follow-up study having a large size of samples collected from equally regional distributions. In conclusion, a more comprehensive approach for improving outcomes in people with both dementia and sensory impairments is needed in the future and further study for developing needed clinical guidelines for all levels of the health care professionals would be a good option and a positive change for better care for the elderly, especially those with dementia.
Acknowledgments
The authors sincerely thank Prof. Piers Dawes, University of Manchester to permit the translation of the K-KAP questionnaire. We also thank Prof. Jin-A Chun, Hallym University to assist collecting our pilot data from the facilities. This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2018S1A3A2074932).
Fig.┬Ā1.
Clinical and subclinical symptoms for older adults who suffer from untreated hearing impairement (top) and dementia (middle). Their common features resulting from less care by the health Table 1. care professionals in their facility (bottom).
Table┬Ā1.
Summary of eight published papers showing the relationship between hearing and/or vision impairment and dementia (or cognitive decline)
| Researcher (year)/Research type | Sample | Assessments | Key findings |
|---|---|---|---|
| Uhlmann, et al. [10] (l99l)/Case-control study | n=174 (each of 87 of cases and a control who had AD and were nondemented, age Ōēź65) | ŌĆó Visual acuity was measured using the Snellen and Rosenbaum method for far and near vision. | ŌĆó The degree of VI significantly correlated with the severity of cognitive dysfunction for both near and far vision. |
| ŌĆó Pure tone audiometry was performed for measuring hearing ability. | ŌĆó VI is associated with both an increased risk and an increased clinical severity of AD, but that increased risk may not be consistent with a progressive dose-response relationship. | ||
| ŌĆó The MMSE score was used as an indicator of cognitive functioning in separate analyses of demented patients. | |||
| Lin, et al. [6] (2004)/Prospective cohort study | n=6,112 of women (aged Ōēź69) | ŌĆó VI was defined as corrected vision worse than 20/40. | ŌĆó A twofold increase in the odds of cognitive and functional decline over time was associated with vision impairment. |
| ŌĆó HL was defined as the inability to hear a tone of 40 dB or greater at 2 kHz. | ŌĆó A trend toward increased odds of cognitive impairment for those with hearing loss at baseline was identified. | ||
| ŌĆó Cognitive and functional decline was defined as 3MS per the National Health Interview Survey Supplement on Aging. | ŌĆó Sensory impairment was associated with cognitive and functional decline in older women. | ||
| Reyes-Ortiz, et al. [8] (2005)/Prospective cohort study | n=2,140 of Mexican Americans (age Ōēź65) | ŌĆó Cognitive function decline was assessed using the MMSE-blind at baseline and at 2, 5, 7 years' follow-up. | ŌĆó Near vision impairment was predictive of cognitive decline in older Mexican Americans independently of other health factors. |
| ŌĆó Visual acuity was measured during an in-home interview. | |||
| ŌĆó Hearing was assessed by the HHIE. | |||
| Lin [4] (2011)/Cross-sectional research | n=605 (ages 60ŌĆō69 year) | ŌĆó HL was defined as the pure-tone average of hearing thresholds. | ŌĆó Greater HL was significantly associated with a lower score on the DSST. |
| ŌĆó Cognitive function was defined by the DSST. | ŌĆó The reduction in cognitive performance associated with a 25 dB HL was equivalent to the reduction associated with an age difference of 6 years. | ||
| ŌĆó HL is independently associated with lower scores on the DSST. | |||
| Lin, et al. [5] (2011)/Original contribution research | n=639 (ages 36ŌĆō90 year) | ŌĆó HL was defined by a PTA at 0.5-4 kHz. | ŌĆó The risk of incident all-cause dementia increases loglinearly with the severity of baseline hearing loss. |
| ŌĆó Incident dementia was diagnosed by a multi-disciplinary consensus diagnostic conference with the standard. | ŌĆó Hearing loss is independently associated with incident allcause dementia. | ||
| Ong, et al. [7] (2012)/Cross-sectional study | n=1,179 (ages 60ŌĆō80 year) | ŌĆó Visual acuity was measured using the logMAR number chart. | ŌĆó Older persons with visual impairment, particularly those with visual impairment due to cataracts, are more likely to have cognitive dysfunction. |
| ŌĆó The Abbreviated Mental Test derived from the Hodkinson Test was used for cognitive function measurement. | ŌĆó Of the major age-related eye diseases, only diabetic retinopathy was associated with cognitive dysfunction. | ||
| ŌĆó Additionally, the major age-related eye diseases (cataracts, glaucoma, diabetic retinopathy, age-related macular degeneration) were considered to be factors for cognitive decline. | |||
| Gurgel, et al. [3] (2014)/Longitudinal cohort research | n=4,463 of the elderly (ages Ōēź65) | ŌĆó 3MS-R was used for a cognitive function comparison. | ŌĆó HL subjects have a higher rate of developing dementia and have more rapid decline than non-HL subjects. |
| ŌĆó HL at baseline was based on observation of hearing difficulties during testing or an interview. | ŌĆó HL was shown to be an independent predictor for developing dementia. | ||
| ŌĆó HL may be a marker for cognitive dysfunction in those 65 years (and older) elderly individuals. | |||
| Thomson, et al. [9] (2017)/Systematic review | n=200-1,338,462 | ŌĆó 17 studies relating HL to dementia or cognitive decline were analyzed. | ŌĆó Although the studies utilized slightly different methods to evaluate the participants, each study demonstrated that hearing loss is associated with a higher incidence of dementia in older adults. |
| ŌĆó The results of the studies were evaluated to determine hearing loss and cognitive status, relevant covariates and confounding factors, and a key finding. |
AD: AlzheimerŌĆÖs disease, VI: vision (or visual) impairment, MMSE: mini-mental state examinations, HL: hearing loss, 3MS: modified mini-mental state examinations, HHIE: hearing handicap inventory for the elderly, DSST: digit symbol substitution test, PTA: pure tone audiometry average, 3MS-R: modified mini-mental state examinations-revised
Table┬Ā2.
Demographic information on study subjects (n=31)
Table┬Ā3.
Sample results for knowledge section gathered from nurse and allied health care professionals (n=4) and caregiver (n=20)
Table┬Ā4.
Sample results from the attitude section for nurse and allied health care professionals (n=4) and caregivers (n=20)
Table┬Ā5.
Sample results for practice section from nurse and allied health care professionals (n=4) and caregivers (n=20)
REFERENCES
1. Korean Statistical Information Service (KOSIS). Population projections and summary indicators (Korea): 2015-2065 [Internet]. Daejeon: KOSIS;2018 [cited 2018 Dec 8]. Available from: URL: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA002&conn_path=I2&language=en.
2. World Health Organization (WHO). Dementia cases set to triple by 2050 but still largely ignored [Internet]. Geneva: WHO;2012 [cited 2019 Jan 9]. Available from: URL: https://www.who.int/mediacentre/news/releases/2012/dementia_20120411/en/.
3. Gurgel RK, Ward PD, Schwartz S, Norton MC, Foster NL, Tschanz JT. Relationship of hearing loss and dementia: a prospective, population-based study. Otol Neurotol 2014;35:775ŌĆō81.



4. Lin FR. Hearing loss and cognition among older adults in the United States. J Gerontol A Biol Sci Med Sci 2011;66:1131ŌĆō6.



5. Lin FR, Metter EJ, OŌĆÖBrien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol 2011;68:214ŌĆō20.



6. Lin MY, Gutierrez PR, Stone KL, Yaffe K, Ensrud KE, Fink HA, et al. Vision impairment and combined vision and hearing impairment predict cognitive and functional decline in older women. J Am Geriatr Soc 2004;52:1996ŌĆō2002.


7. Ong SY, Cheung CY, Li X, Lamoureux EL, Ikram MK, Ding J, et al. Visual impairment, age-related eye diseases, and cognitive function: the Singapore Malay Eye study. Arch Ophthalmol 2012;130:895ŌĆō900.


8. Reyes-Ortiz CA, Kuo YF, DiNuzzo AR, Ray LA, Raji MA, Markides KS. Near vision impairment predicts cognitive decline: data from the Hispanic Established Populations for Epidemiologic Studies of the Elderly. J Am Geriatr Soc 2005;53:681ŌĆō6.


9. Thomson RS, Auduong P, Miller AT, Gurgel RK. Hearing loss as a risk factor for dementia: a systematic review. Laryngoscope Investig Otolaryngol 2017;2:69ŌĆō79.



10. Uhlmann RF, Larson EB, Koepsell TD, Rees TS, Duckert LG. Visual impairment and cognitive dysfunction in AlzheimerŌĆÖs disease. J Gen Intern Med 1991;6:126ŌĆō32.



11. Horowitz A. The prevalence and consequences of vision impairment in later life. Top Geriatr Rehabil 2004;20:185ŌĆō95.

12. Strawbridge WJ, Wallhagen MI, Shema SJ, Kaplan GA. Negative consequences of hearing impairment in old age: a longitudinal analysis. Gerontologist 2000;40:320ŌĆō6.



13. Schopper D, Doussantousse S, Orav J. Sexual behaviors relevant to HIV transmission in a rural African population. How much can a KAP survey tell us? Soc Sci Med 1993;37:401ŌĆō12.









