Approaching Knowledge, Attitudes, and Practices Model for Elderly with Dementia Who are Suspected to Have Hearing Impairment in Korea
Article information
Abstract
Because the psychophysical symptoms of hearing loss and dementia in the elderly are very similar, untrained healthcare professionals in dementia facilities can easily overlook a severity of hearing loss in their patients. The present study identifies their knowledge, attitudes, and practices (KAP) on hearing loss using a survey whether they may help hearing problem of the patients with dementia. A total of 29 health-care professionals responded to the KAP survey. Also, 2 family members participated. The results showed that most of the nurses and caregivers in elderly medical welfare facilities who worked with dementia patients did not have knowledge of their hearing loss. Even the facility managers did not know how to conduct hearing tests for their patients although they did recognize that some of their patients had a hearing loss. Eventually, actual practice was not possible at this moment by the professionals. However, our respondents did have a positive attitude toward screening for hearing loss and help their patients with dementia wear hearing aids if a clinical guideline was provided. We suggest to develop clear and precise clinical guidelines of the hearing screening test for the dementia patients due to the interrelationship between dementia and hearing loss. When these guidelines apply to elderly residents in a medical welfare facility, early diagnosis and treatment of their sensory loss will help alleviate their dementia as well.
Introduction
Since improved surgical procedures and treatment techniques have made it possible to overcome various maladies, the human life span has been extended; thus, the number of older adults is increasing globally. South Korea is also showing the same unprecedented rapid aging trend. According to the report by Korean Statistical Information Service, its ratio of elderly population will reach 20% of total population in 2025, making Korea a super-aged society [1]. Thus, common chronic diseases of the elderly are currently considered carefully at the government level, along with a need for better care of the elderly.
The elderly with dementia is globally estimated at 35.6 million as of 2012 and forecast to triple by 2050 [2]. Given that new attention, there is strong evidence that the degraded functioning of aging sensory systems may be associated with cognitive decline in the elderly. Contemporary researchers have thus investigated the relationship between hearing and/or vision impairments of old adults and cognitive dysfunction. As examples, we summarize here eight well-designed studies [3-10] in Table 1. Although the methodology applying for functional and dysfunctional measurements of the sensory and cognitive systems were slightly different across these studies [3-5,9], all concluded that either hearing or vision loss in the older population could fatally affect any dementia. In particular, the symptoms caused by untreated hearing loss showed very similar tendencies for worsening cognitive decline or dementia, while limiting social activity and producing isolation, depression, a lower quality of life, and reduced mental well-being overall [11,12].

Summary of eight published papers showing the relationship between hearing and/or vision impairment and dementia (or cognitive decline)
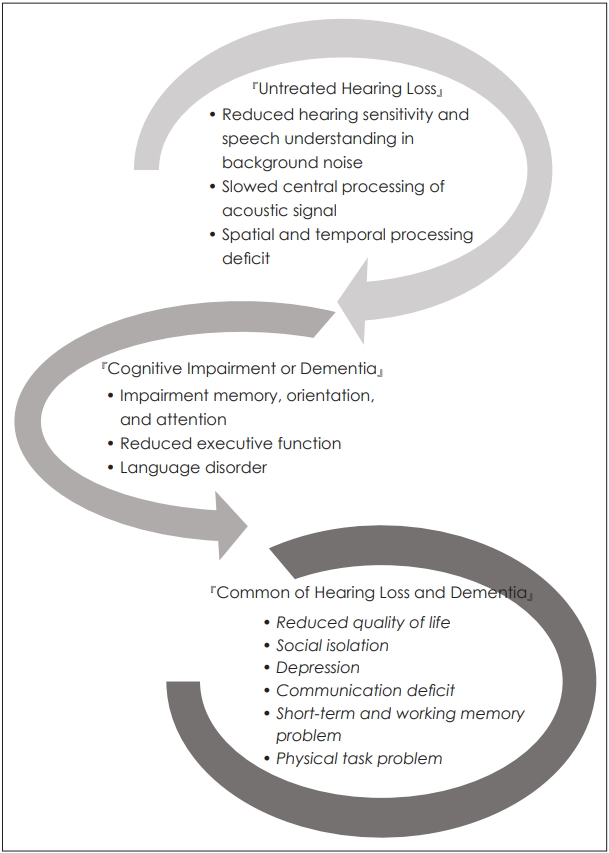
Although each case of hearing loss and cognitive impairment can have a different characteristic due to the different sites of the lesion, i.e., the ear and brain, respectively, Fig. 1 demonstrates that the two diseases share many common psychophysical symptoms, including a lower quality of life, communication disability, social isolation, depression, and more. In other words, any patient who suffers from both dementia and hearing loss, the symptoms of hearing loss may be confusable or covered up as part of the cognitive impairment, thereby resulting in their hearing system remaining untreated. When considering the increased risks for dementia and the significant negative impact of comorbidity of two diseases on the mental well-being of the elderly, it becomes even more necessary to clinically evaluate the hearing loss in dementia patients.
On the other hand, the Knowledge, Attitudes, and Practices (KAP) survey is a representative tool used for a specific population to collect information on what is known, believed, and done in relation to a specific field. Historically, the KAP model was developed for family planning and population studies in the 1950s, with its purpose being to measure the extent to which any clear opposition to the notion and organization of family planning existed among different populations, so specific family planning practices could be used for different program purposes worldwide. In the 1960s and 1970s, the number of studies on community perspectives and human behavior grew rapidly in response to the needs of the primary health care approach that was adopted by international aid organizations [13]. Since that time, these KAP surveys had been used to investigate health behavior and continued to be widely used to gain information on health-seeking practices. Based on the KAP model, knowledge affects attitude and practice directly, and attitude will also directly affect actual practice or intentions [14]. In other words, three factors were related and thus considered together.
This brief communication identifies KAP on hearing loss of the health-care professionals in the elderly medical welfare facilities, while using a questionnaire based on that KAP model. Also, as an early stage of approach, we discuss what can be provide for them and their patients by hearing professionals in Korea
Subjects and Methods
Survey items
To develop the Korean version of KAP (K-KAP) survey, a questionnaire was adapted [15] with both translation and back-translation from English to Korean by a professional translator, and inappropriate questions related to the Korean health system were modified (i.e., the residential aged care setting in the original version of the KAP survey was modified to be an elderly medical welfare facility and long-term hospitalized facility). The final version of the questionnaire was consulted on and confirmed by professors with long careers in the Audiology and Nursing fields.
The K-KAP survey consisted of four target populations for each version: 1) Facility Manager (46 questions), 2) Nurses and Allied Health Professionals (25 questions), 3) Caregivers (25 questions), and 4) Family Members of Patients (19 questions). The version for facility workers (1 to 3) investigated three aspects of knowledge, attitudes, and practices- related sensory impairments for dementia, while the version of family members included several questions about sensory loss of their patients at the facility. Each version of the questionnaire had the same purpose, but it was slightly different in terms of its scope of gathered information. For example, the version for the facility manager included questions on whether employees were educated for related sensory impairment for patients with dementia, how to reflect support of the management plan, and more. The version for the nurses and allied health professionals and caregivers included questions on whether they had received education about sensory loss and the interpretation of results of screening tests. In other words, the questionnaire was systematically structured in terms of each participant’s position and related circumstances.
Participants
Before extending in a larger scale study in Korea, participants were randomly contacted to two facilities, one for Namyangju city and the other for Chuncheon city in easy accessibility and short duration of the pilot study. The target participants consisted of four groups’ working at legally designated ‘elderly medical welfare facilities’ and a ‘long-term hospitalized facility (in Korea, the elderly medical welfare facility provides nursing and assisting other daily life for the elderly, whereas the long-term hospitalized facility has a similar service except for professional medical services to patients by doctors and nurses)’ in Korea and these facility patients’ family member.
For the sample data, a total of 31 subjects completed a questionnaire with a sufficient explanation of its purpose and method. The respondents consisted of 4 facility managers, 5 nurses and allied health professionals, 20 caregivers, and 2 family members of patients. Detailed information on the respondents is included in Table 2.
All procedures for the present study were approved by Hallym University’s Institutional Review Broad (HIRB-2018-065) and the participants were asked to sign an informed consent before they completed the questionnaire.
Results
Facility managers
Five facility managers who have worked for nearly two years responded and recognized that a number of the dementia patients with sensory loss and the degree of their loss (4 out of 5). However, none responded and indicated they know how to screen for difficulty of hearing or vision for their patients. In terms of attitude, three out of five managers were able to test the hearing or vision when provided with specific clinical guidelines (or a program manual) and screen their patients’ sensory systems. Although most of the managers did not know the guidelines well, they were positive about monitoring the hearing or vision conditions of their patients and recognized it was as necessity. Nevertheless, current situation indicated that there was no facility or staff training on doing hearing and/or vision tests as a typical practice.
Nursing and allied health staff
Table 3 displays the responses from 4 nurse and allied health care professionals and 20 caregivers on their knowledge. Although 3 out of 4 nurses partially knew their patients had hearing or vision loss and the way to use to refer them to professionals, they could not conduct simple testing (100%) and also not interpret the results (75%) due to a lack of training and/or knowledge. Thus, they also reported having less confidence in handling assistive devices for hearing and vision. Compared to the responses of the nurses, the answers of caregivers were less knowledgeable and seemed negative.

Sample results for knowledge section gathered from nurse and allied health care professionals (n=4) and caregiver (n=20)
Regarding attitudes on the KAP survey (Table 4), the respondents partially agreed with conducting screen tests for hearing or vision. In particular, the caregivers wanted more guidance about the clinical guidelines. Also 80% of the caregivers reported that their patients with dementia might actually use hearing aids effectively. In Table 5, our respondents report that most did not test or check the assistive devices of hearing and vision, such as hearing aids and spectacles, while also having no opportunity to be educated or training. There was no specialized staff to care the hearing or vision loss for their patients.

Sample results from the attitude section for nurse and allied health care professionals (n=4) and caregivers (n=20)
Family members
Although there was a very small sample size, family members also reported that they knew their mothers had a hearing loss, but they did not try to ask for hearing screening or care or hearing aids for her because the staffs at the facility were untrained.
Conclusions and Further Implication
The present study surveyed KAP of staffs in the aged care facility and of family members of residents towards hearing and identified any feasibility of K-KAP survey to find any relation of three factors. The current pilot data showed that most respondents who were nurses and caregivers in the elderly medical welfare facility and had worked for dementia patients did not have any/enough knowledge of the hearing loss of the elderly. Even the facility managers did not know about how to conduct hearing tests for their patients although they did realize that some of their patients had hearing loss. Thus, the practice, e.g., test and interpretation of those results and checking an assistive device, was not possible in the current situation. However, our respondents did some positive attitudes toward screen for hearing loss and helping elderly with dementia wear their hearing aids if specific clinical guidelines were provided.
Although we consider that direct support of hearing and vision impairments, by fitting hearing aids and eye glasses, is unlikely to succeed in the context of more serious cognitive deficits, such as dementia, and many do think about the complexity of concurrent deficits as well as the low rate of access to vision and hearing services in many elderly people, the related studies have proven that untreated hearing loss negatively affects dementia. Although the current data was only a small sample and limited to a specific regional area, there is a lack of systematic care for dementia patients with hearing loss in Korea, which warrants a follow-up study having a large size of samples collected from equally regional distributions. In conclusion, a more comprehensive approach for improving outcomes in people with both dementia and sensory impairments is needed in the future and further study for developing needed clinical guidelines for all levels of the health care professionals would be a good option and a positive change for better care for the elderly, especially those with dementia.
Acknowledgements
The authors sincerely thank Prof. Piers Dawes, University of Manchester to permit the translation of the K-KAP questionnaire. We also thank Prof. Jin-A Chun, Hallym University to assist collecting our pilot data from the facilities. This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2018S1A3A2074932).
Notes
Conflicts of interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Sunghwa You and Woojae Han. Formal analysis: Sunghwa You. Funding acquisition: Woojae Han. Project administration: Woojae Han. Visualization: Sunghwa You. Writing—original draft: Sunghwa You. Writing—review & editing: Woojae Han.