Introduction
Trichofolliculomas (TFs) are rare adnexal tumors, reported as hamartomatous tumors or as benign follicular neoplasms, commonly affecting the head and neck regions. However, auricular involvement is extremely rare, and to the authorŌĆÖs best knowledge, only 2 cases of ear or ear canal TF has been described in the English literature [1,2]. These benign hair follicle-derived tumors may clinically mimic malignancy such as basal cell carcinoma of the auricle. Histopathological examination is most often required to confirm the diagnosis. Complete excision of the tumor is the treatment of choice, as remnants of the lesion can lead to recurrence despite its benign nature [3]. Herein, the author describes a rare case of a TF arising from the auricle and review the relevant literature.
Case Report
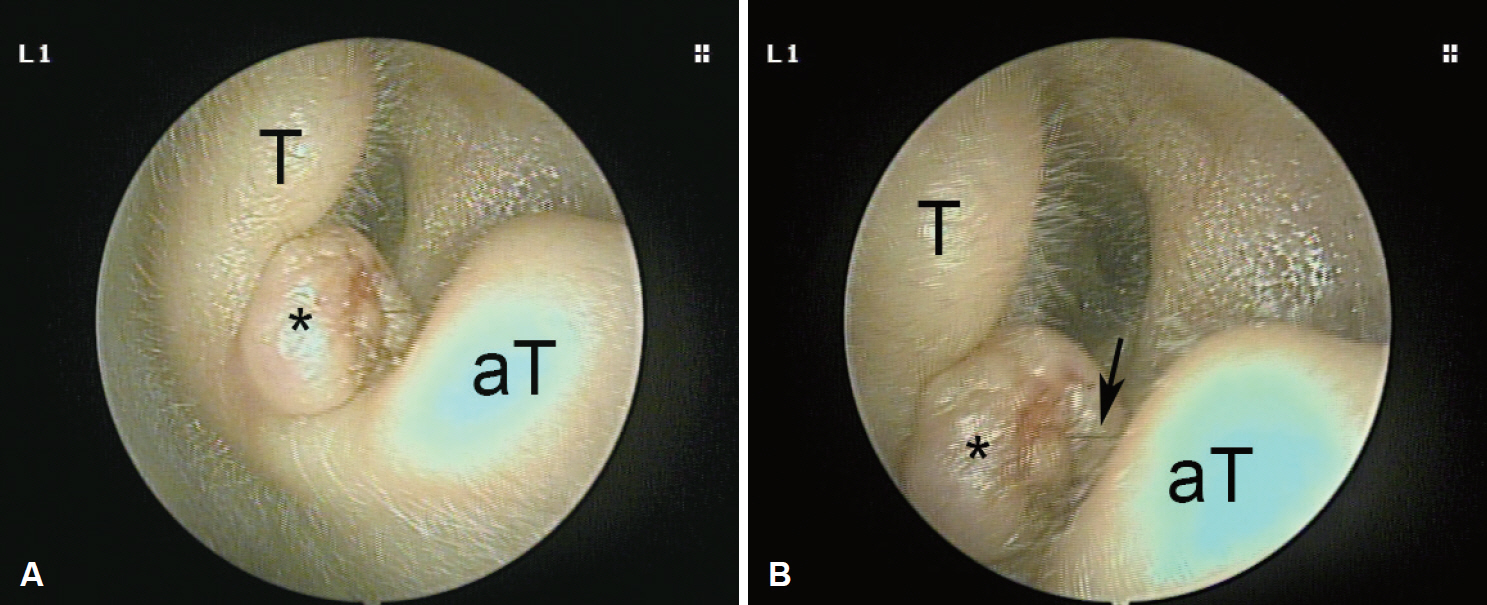
A 48-year-old female patient presented with a several-year history of a slowly increasing asymptomatic mass in the lateral surface of the left auricle, near the concha. The patient could not recall any history of trauma at the site of swelling. The lesion appeared as a solitary 0.8 cm skin-colored, dome-shaped nodule with irregular borders. In detail, the round mass had central small pitted umbilication and a tuft of fine hair protruding out of it (Fig. 1). In palpation, it was smooth, rubbery to firm in consistency, and fixed to the the intertragal notch of the left auricle without cartilage component. The remainder of the physical examination was unremarkable. There were no local lymphadenopathy and any other masses in the body in physical examination. Clinical diagnosis of accessory tragus, hair follicle nevus, other adnexal tumor, and basal cell carcinoma were also made due to irregular surface.
Because the patient wanted to remove the mass, wide local excision was planned. The mass was removed completely. Intraoperatively, it was adherent to the auricular epidermis so that it was inevitable to expose the auricular perichondrium. After removal of the mass, the exposed wound and perichondrium was covered with split-thickness skin graft. The biopsied tissue was single, firm, globular grey white and measured 0.6├Ś0.5├Ś0.5 cm in size.
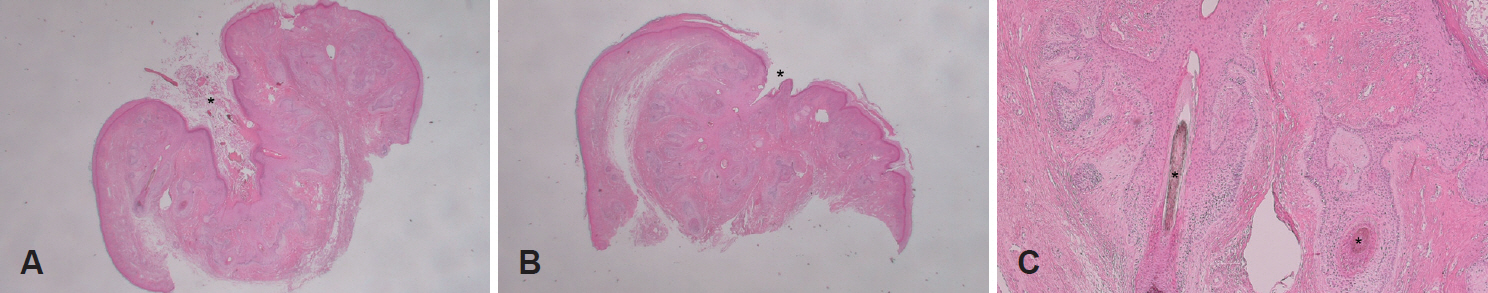
Histopathological examination showed a dilated central cystic follicle that communicated with the overlying skin surface. The dilated follicular opening showed keratin debris and hair. The follicle was lined with squamous epithelium and surrounded by numerous smaller secondary follicles, many of which contained fragments of hair shafts along with many variables sized hair follicles exhibiting varying degree of maturation (Fig. 2). Epidermis and dermis unremarkably showed strands of stratified squamous epithelium. Many fibroblasts was observed at the the stroma. The histopathological analysis was consistent with TF. There was no recurrence after a follow up of 1 year.
Discussion
The TF is a rare adnexal hamartoma of the skin with differentiation to hair follicles [4]. The TF is found mostly in adults as a fresh-colored solitary nodule at the face and scalp [4]. Rarely, the external auditory canal, intranasal area, lip, and vulva are affected [5]. No definitive racial and sexual predilection is reported.
The TF is clinically characterized by a small, asymptomatic, skin colored dome shaped nodule with a central pore, through which a small tuft of one or two hairs protrude. Sometimes, the pore of the nodule appears as a black spot. If the hair has been plucked or is too fine and ignored during examination, the growth may mimic basal cell carcinoma or molluscum contagiosum. Furthermore, if a dilated central cystic follicle is missed on histological sections, and the secondary follicles fail to show any hair structures, then the lesion may misdiagnosed as a trichoepithelioma or even basal cell carcinoma.
TF was first described by Miescher [6] in 1944 as a nodule with a central large pore from which a tuft of hairs protruding. In 1957, Hyman and Clayman [7] reported a similar case and labeled it a ŌĆ£hair follicle nevus.ŌĆØ However, Kligman and Pinkus [8] suggested the term ŌĆ£folliculoma,ŌĆØ as it differs from a nevus by the presence of hair follicle.
The etiology of TF is uncertain, onset is usually spontaneous. However, history of previous trauma has been reported [9]. TF is cosmetically disfiguring and patients may tend to pluck out the hair emerging from it, which sometimes may lead to an inflammatory reaction. There are no any reports for relating systemic or skin disorders and they are considered as an abortive differentiation of pluripotent skin cells toward hair follicles.
According to Kligman and Pinkus [8], it shows intermediate differentiation between a hair follicle nevus, which is simple hyperplasia of the hair follicle, and a trichoepithelioma, which usually lacks a mature hair follicle. It might be also misdiagnosed as sebaceous cyst, nevus, molluscum contagiosum, or even basal cell carcinoma, especially when the hair has been missed [9].
Histopathological examination is mandatory to confirm the diagnosis. Definite clue is a stratified squamous epithelium lined cystic follicle that communicated with the overlying skin surface. Many secondary follicles can be observed around the central cystic follicle. Scanty lymphocytic or graulomatous inflammation might be observed. Within the follicular epithelium, many merkel cells have been present, supporting that TFs are hamartomas. In addition, it can be subdivided into three stages, which are early, fully developed, and late stage [10]. In early stages, there are few secondary hair follicles originating from a primary one. In very early stages, it may mimic trichoepithelioma, dermal nevus, or epidermoid cyst if the pore is not clearly visible. In mature lesions, vellus hair follicles increase in number. Later stages show a thickened primary follicle and fewer secondary follicles [9]. The evolution of TF is considered similar to a regressing normal hair follicle but probably in a one way direction with no regeneration from telogen to anagen.
TF is considered a benign entity, despite one case report of malignant transformation with perineural invasion [11]. Local excisional biopsy is diagnostic and further treatment may not be needed.
Histologically, hair follicle nevus and accessory tragi are the most difficult to distinguish of the lesions in the differential diagnosis of TFs. Their histologic backgrounds are very similar except the amounts of hair follicles and subcutaneous fat [12]. TF is a pilar tumor and intermediate in differentiation between a trichoepithelioma, which misses maturation of the hair follicle and a hair follicle nevus, which is simple hyperplasia of the hair follicle. On the other hand, central cyst and radiating hair follicles are much found in the TF.
Accessory tragus is a more complex structure, which consists not only of a pilar complex but also cutaneous appendages in different stages of development. A central cartilage structure is present in most accessory tragi. Many authors have stated that accessory tragi and hair follicle nevi are on the same spectrum. Asahina, et al. [13] stated that, although this may be the case, the developmental mechanisms might vary according to the location or component of the lesion.
Satoh, et al. [14] reported the accessory tragi had a prominent connective tissue in subcutaneous fat. In contrast, Ban, et al. [15] explained that a connective tissue framework in subcutaneous fat appears in both hair follicle nevus and accessory auricle, and that the accessory auricle can be differentiated by the presence of abundant, subcutaneous fat.
When a lesion located in a preauricular area at birth or when it contains cartilage part, we may call it accessory tragus. In contrast, a lesion occurs in an atypical area for accessory tragus, and miss cartilage and is then interpreted as hair follicle nevus.
Treatment of TF is usually not required. At times, TF may be disfiguring, and the pulling away of hairs and other injuries may cause inflammatory reactions requiring treatment. In such cases and for the confirmative diagnosis, surgical excision is usually inevitable and recommendable. The prognosis is excellent, although recurrence can occur at the primary site rarely [3].
In conclusion, TF is a benign nodular hamartoma, rarely involving the auricle. Although rare, it should be considered in the differential diagnosis in all cases of asymptomatic, fleshcolored, dome shaped, solitary auricular nodule with a central pit and tufts of hairs. Complete excision of the tumor is the treatment of choice, and incomplete excision may lead to recurrence.