|
 |
- Search
| J Audiol Otol > Volume 26(3); 2022 > Article |
|
Abstract
Background and Objectives
We investigated the clinical validity of and correlation between the Eustachian Tube Dysfunction Questionnaire-7 (ETDQ-7) scores and the eustachian tube function test (ETFT) results in patients with a normal drum.
Subjects and Methods
The study included 49 patients (93 ears) with unilateral or bilateral ear fullness over >3 months. All patients were administered the ETDQ-7 survey and underwent the ETFT on the same day. The receiver operating characteristic (ROC) curve and the association between the results were statistically analyzed.
Results
ETDQ-7 scores were not significantly correlated with the ETFT results or with middle ear pressure. ETDQ-7 scores in patients with eustachian tube dysfunction (ETD) were significantly higher than those in patients with normal ETFT results (p=0.039) when ETD was defined as a pressure change <10 daPa on the ETFT. The area under the ROC curve was 0.631, with a sensitivity of 37.0% and specificity of 89.4%.
The eustachian tube is the only conduit connecting the middle ear cavity and the nasopharynx, and it plays several roles in maintaining middle ear health. It has a ventilation function that equalizes the pressure between the middle ear and the atmosphere, a drainage function that excretes secretion from the middle ear into the nasopharynx, and a defensive function that prevents reflux from the nasopharynx [1-6]. It is generally accepted that eustachian tube dysfunction (ETD) is associated with several middle ear diseases [7,8]. Further, improper opening of the eustachian tube, such as owing to obstructive ETD, can cause miscellaneous ear symptoms, including ear fullness, popping sound, and otalgia [4,9-11].
The quantitative evaluation of eustachian tube function is challenging. Classically, the Valsalva maneuver, Toynbee maneuver, Frenzel maneuver, and Politzer maneuver can readily be conducted in the office [12]. However, specific devices are required to quantitatively measure eustachian tube function. Sonotubometry and tubomanometry are representative methods to evaluate eustachian tube function that can quantitatively measure it [13-17]. Bluestone’s nine-step test and inflation/ deflation test can also evaluate physiologic function induced by swallowing [18,19]. In addition, Bluestone’s nine-step test is a simple test based on impedance audiometry for patients with the normal drums. However, there is no single gold-standard test to evaluate eustachian tube function that is universally accepted [20,21].
Since 2012, the Eustachian Tube Dysfunction Questionnaire-7 (ETDQ-7), which was introduced by McCoul et al. [9] has been widely used to quantify the subjective symptoms of ETD. The ETDQ-7 is a disease-specific instrument that has reported 100% sensitivity and specificity in cut-off average score 2.1 in patients with ETD who had abnormal tympanometry. Similarly designed studies using translated versions of ETDQ-7 have also reported >90% sensitivity and specificity [22-25]. However, unlike these studies enrolled patients having abnormal tympanometry as an ETD group, ETD is often diagnosed by representative symptoms alone, without the abnormal drum findings [11, 26-28].
Therefore, it is necessary to clarify the relationship between symptom-based ETDQ-7 and the objective eustachian tube function test (ETFT) in patients with normal drum. This study retrospectively analyzed the result of ETDQ-7 and ETFT using GSI TympStar Pro (Grason-Stadler Inc., Eden Prairie, Minnesota, MN, USA) from all patients who had ear fullness in at least one ear with a normal tympanic drum. We expect that this study will reveal the clinical value of ETDQ-7 in the real world, possibly helping clinicians in the selection of candidates for surgical intervention.
We retrospectively reviewed medical records from May 2021 to Aug 2021 to identify patients 1) who complained of ear fullness for more than 3 months without patulous eustachian tube symptoms such as autophony or breathing sounds, and 2) with normal drum findings. Patients were excluded if they had the result of impedance audiometry type B (absence of peak impedance) or were under the age of 12 years. Based on these criteria, a total of 93 ears of 49 patients were included. The ETDQ-7 survey and ETFT were routinely conducted in patients who complained of ear fullness; thus, all enrolled patients had the results of these examinations. The institutional review board of the Severance Hospital approved this study, and the need for informed consent was waived owing to the retrospective design of the study (4-2021-1180).
All enrolled patients underwent a Korean language version of the ETDQ-7 survey and ETFT using GSI TympStar Pro (Grason-Stadler Inc.) on the same day. The ETDQ-7 consisted of seven questionnaires that included representative symptoms of ETD. ETFT by GSI TympStar Pro (Grason-Stadler Inc.) is based on Bluestone’s nine-step test. Initially, the middle ear pressure was evaluated in a normal state. Next, 400 daPa of negative pressure was introduced to the ear canal, followed by dry swallowing thrice, after which the middle ear pressure was evaluated. Lastly, the same procedure was performed using 400 daPa of positive pressure. The maximal difference in eustachian tube function test (ETFTMD) from the three states is regarded as the reflection of eustachian tube function. According to the manufacturer’s guidelines, more than 15 daPa of maximal difference is regarded as normal. However, suggested maximal difference is more than 10 daPa after the Valsalva manuver as a normal cut-off value. Therefore, the authors analyzed both of cut-off values (ETFT <10 and ETFT <15). The receiver operating characteristic (ROC) curve and the relationship between the results were statistically analyzed.
We examined the correlation between the results using Spearman’s rho. Student’s t-test was used to compare the two groups. The ROC curve was visualized using Prism 8.0 (GraphPad Software, San Diego, CA, USA). The sensitivity and specificity were evaluated from the ROC curve. All statistical analyses were conducted using IBM SPSS version 20 (IBM Co., Armonk, NY, USA), and p<0.05 was considered statistically significant.
A total of 93 ears of 49 patients aged 15-74 years (mean, 41.00±17.22 years) were included in this study; 14 (28.6%) were male (Table 1). The mean score of ETDQ-7 was 2.75±1.19, and 32 ears scored less than 2.1. The group with ETD was defined by the maximal difference in middle ear pressure in the ETFT; two cut-off values were evaluated. There were 27 diseased ears (29.0%) with ETFT <10 daPa and 36 ears (38.7%) with ETFT <15 daPa. Normal middle ear pressure and peak impedance were -8.74±29.13 daPa and 0.70±0.81 mmho, respectively.
The results of ETFTMD and ETDQ-7 did not show a significant correlation (r=-0.032, p=0.764) (Table 2). Furthermore, none of the individual scores of the questionnaire showed a significant correlation with ETFTMD. ETDQ-7 did not show a significant correlation with any other factor, including middle ear pressure and peak impedance. Conversely, ETFTMD showed a significant positive correlation with middle ear pressure (r=0.358, p<0.001) (Fig. 1). This implies that middle ear pressure tends to be negative in patients with poor eustachian tube function.
When ETD was defined as ETFTMD <15 daPa, the area under the curve (AUC) of ETDQ-7 was 0.562 (p=0.317) (Fig. 2). The sensitivity and specificity of the mean ETDQ-7 cut-off of 4.07 was 25.0% and 91.2%, respectively. In addition, the questionnaires in ETDQ-7 did not show a significant difference between the ETD group and the normal group (Table 3).
In contrast, when ETD was defined as ETFTMD <10 daPa, the AUC of ETDQ-7 was 0.631 (p=0.049). The sensitivity and specificity of the mean ETDQ-7 cut-off of 3.93 was 37.0% and 89.4%, respectively. The scores of questionnaire 2 (p=0.039), 6 (p=0.039), 7 (p=0.011), and mean ETDQ-7 (p=0.039) were significantly higher in the ETD group.
In our cohort of patients with ear fullness with a normal drum, the ETDQ-7 and ETFT results did not show a significant correlation. Furthermore, when ETD was defined as ETFTMD <10 daPa, the sensitivity and specificity of ETDQ-7 were 37.0% and 89.4%, respectively, with an AUC of 0.631. This is an unexpectedly poor outcome compared to the previous outcomes of ETDQ-7 in case-control studies. ETDQ-7 is reported to have a sensitivity of 91%-100% and specificity of 67%-100% [22-24,29]. However, these were case-control studies, and the case group was defined as those who had ETD symptoms and a tympanic membrane abnormality detected by an otoscope or an abnormal impedance audiometer. Consequently, our result might underestimate the clinical value of ETDQ-7 because our cohort only included patients with normal drums. However, patients with ETD with normal tympanometry and normal drum also exist, which can make the decision to intervene difficult. Indeed, in a randomized controlled study by Meyer et al. [11], 51% of patients with ETD (mean ETDQ-7 >3.0) showed a normal tympanic membrane position, and 71.3% had normal tympanometry. After eustachian tube balloon dilation, their symptoms dramatically improved regardless of tympanometry or the tympanic membrane position [11]. This implies that clinicians might overlook a treatable patient if they consider only surgical candidates with abnormal tympanometry or drum.
To address this, several methods were suggested. Recently, the eustachian tube score (ETS-7), which showed 96% sensitivity and 97% specificity for distinguishing patients with chronic ETD, was reported [30]. ETS-7 is based on tubomanometry, swallowing click sound, and Valsalva test. Interestingly, this scoring system also showed a poor AUC in ROC analysis (0.64) when compared to ETDQ-7. In our result, ETFTMD <10 showed a significant AUC in ROC analysis (0.631). In addition, ETDQ-7 does not correlate with ETFT or results of tympanometry. Taken together, the clinical value of ETDQ-7 appears unsatisfactory if it is solely conducted. Although ETDQ-7 is still a good measurement for subjective ETD symptoms, an objective test should be co-conducted to narrow the diagnostic criteria.
The ETFT using commercial GSI TympStar Pro (GrasonStadler Inc.) is a simple tool to evaluate the eustachian tube during swallowing in patients with a normal drum. The manufacturer’s guidelines indicate that the normal value of ETFTMD is >15 daPa. However, there is a lack of studies comparing this instrument with other test modalities such as sonotubometry and tubomanometry. Based on our results, ETFTMD showed a significant correlation with the middle ear pressure in tympanometry. Given that negative middle ear pressure results from the gas exchange of capillary blood flow of middle ear mucosa when the ventilation is disrupted owing to ETD, significant negative correlation of ETFTMD and middle ear pressure (r=0.358, p<0.001) is plausible [31-33]. Based on our results, the ETFTMD cut-off value of 10 daPa better reflects the severity of symptoms in patients with ETD and normal drum.
This study has some limitations. First, the Korean version of ETDQ-7 has never been statistically validated. Second, all enrolled patients had ear fullness in at least one ear, thus a healthy control was substituted by an asymptomatic ear of patients. This may result in underestimation of the sensitivity and specificity of ETDQ-7. Third, other modalities for measuring eustachian tube function, such as tubomanometry and ETS-7, were not conducted. ETFTMD alone may not be accurate enough to diagnose ETD.
In conclusion, based on our result that ETDQ-7 is not well correlated with ETFT, the results of ETDQ-7 may largely be affected by subjective symptoms. Therefore, ETDQ-7 should be co-conducted with objective tests to evaluate eustachian tube function. In addition, ETFTMD <10 daPa can be used to objectively evaluate eustachian tube function.
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2020R1I1A1A01067241 to S.H. Bae).
Notes
Author Contributions
Conceptualization: Seong Hoon Bae, In Seok Moon, Jinsei Jung. Data curation: Seojin Moon, Yujin Lee. Formal analysis: Seojin Moon. Funding acquisition: Seong Hoon Bae. Methodology: Seong Hoon Bae, In Seok Moon, Jinsei Jung. Project administration: Seong Hoon Bae. Visualization: Seojin Moon, Yujin Lee. Writing—original draft: Seojin Moon, Seong Hoon Bae. Writing—review & editing: Seong Hoon Bae. Aproval of final manuscript: all authors.
Fig. 1.
Correlation between middle ear pressure (MEP) and maximal difference in eustachian tube function test (ETFTMD). The hollow circles indicate each patient. The black line indicates correlation slope.
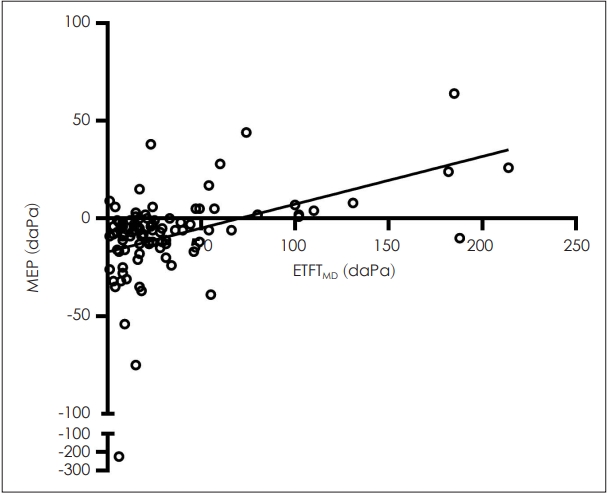
Fig. 2.
Receiver operating characteristic curve with Eustachian tube function test (ETFT) as a reference. A: ETFT <10 daPa as a reference. B: ETFT <15 daPa as a reference.
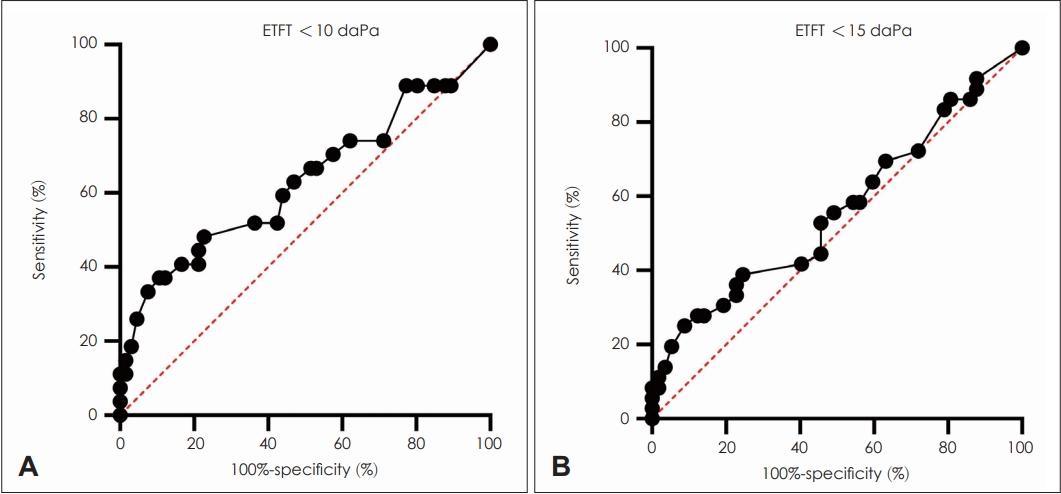
Table 1.
Patient information (93 ears of 49 patients)
Table 2.
Correlation between ETDQ-7 and ETFTMD
| ETDQ-7 | ETFTMD | MEP | Imp | ||
|---|---|---|---|---|---|
| ETDQ-7 | r | 1 | - | - | - |
| p-value | N/A | - | - | - | |
| ETFTMD | r | -0.032 | 1 | - | - |
| p-value | 0.764 | N/A | - | - | |
| MEP | r | -0.177 | 0.358* | 1 | - |
| p-value | 0.090 | <0.001 | N/A | - | |
| Imp | r | 0.074 | 0.162 | 0.156 | 1 |
| p-value | 0.484 | 0.122 | 0.136 | N/A |
Table 3.
Analysis of ETDQ-7 results based on abnormal ETFT
|
ETFT <15 daPa as a reference |
ETFT <10 daPa as a reference |
|||||
|---|---|---|---|---|---|---|
| ETFT <15 | ETFT ≥15 | p-value | ETFT <10 | ETFT ≥10 | p-value | |
| Ears | 36 | 57 | 27 | 66 | ||
| ETDQ-7 | 3.0±1.4 | 2.6±1.1 | 0.170 | 3.2±1.4 | 2.6±1.0 | 0.039* |
| Q1 | 4.1±2.0 | 3.7±1.8 | 0.333 | 4.2±2.0 | 3.7±1.8 | 0.185 |
| Q2 | 2.2±1.5 | 1.9±1.4 | 0.420 | 2.5±1.6 | 1.8±1.3 | 0.039* |
| Q3 | 3.9±2.0 | 3.8±1.9 | 0.912 | 4.0±2.0 | 3.8±2.0 | 0.664 |
| Q4 | 2.4±1.8 | 2.5±1.8 | 0.862 | 2.7±1.9 | 2.3±1.8 | 0.353 |
| Q5 | 2.6±2.0 | 2.1±1.7 | 0.209 | 2.9±2.1 | 2.1±1.7 | 0.085 |
| Q6 | 3.2±2.0 | 2.5±1.8 | 0.086 | 3.4±2.2 | 2.5±1.7 | 0.039* |
| Q7 | 2.4±1.7 | 1.8±1.2 | 0.053 | 2.7±1.8 | 1.7±1.1 | 0.011* |
| MEP | -19.3±39.0 | -2.1±18.0 | 0.005* | -22.0±42.9 | -3.3±19.0 | 0.004* |
| IMP | 0.6±0.4 | 0.8±1.0 | 0.233 | 0.6±0.4 | 0.7±0.9 | 0.501 |
REFERENCES
1. Bluestone CD, Doyle WJ. Anatomy and physiology of eustachian tube and middle ear related to otitis media. J Allergy Clin Immunol 1988;81(5 Pt 2):997–1003.


3. Sadé J, Ar A. Middle ear and auditory tube: middle ear clearance, gas exchange, and pressure regulation. Otolaryngol Head Neck Surg 1997;116:499–524.


4. Schilder AG, Bhutta MF, Butler CC, Holy C, Levine LH, Kvaerner KJ, et al. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol 2015;40:407–11.




5. Smith ME, Scoffings DJ, Tysome JR. Imaging of the eustachian tube and its function: a systematic review. Neuroradiology 2016;58:543–56.




6. Alper CM, Luntz M, Takahashi H, Ghadiali SN, Swarts JD, Teixeira MS, et al. Panel 2: anatomy (eustachian tube, middle ear, and mastoid—anatomy, physiology, pathophysiology, and pathogenesis). Otolaryngol Head Neck Surg 2017;156(4_suppl):S22–40.



7. Seibert JW, Danner CJ. Eustachian tube function and the middle ear. Otolaryngol Clin North Am 2006;39:1221–35.


8. Sente M. [Importance of the eustachian tube in middle ear function]. Med Pregl 1995;48:405–6. [Article in Croatian].

9. McCoul ED, Anand VK, Christos PJ. Validating the clinical assessment of eustachian tube dysfunction: the eustachian tube dysfunction questionnaire (ETDQ-7). Laryngoscope 2012;122:1137–41.



10. Hamrang-Yousefi S, Ng J, Andaloro C. Eustachian tube dysfunction. Treasure Island, USA: StatPearls Publishing;2022.
11. Meyer TA, O’Malley EM, Schlosser RJ, Soler ZM, Cai J, Hoy MJ, et al. A randomized controlled trial of balloon dilation as a treatment for persistent eustachian tube dysfunction with 1-year follow-up. Otol Neurotol 2018;39:894–902.



12. Bluestone CD, Cantekin EI. Current clinical methods, indications and interpretation of eustachian tube function tests. Ann Otol Rhinol Laryngol 1981;90(6 Pt 1):552–62.



13. Olander H, Järnstedt J, Poe D, Kivekäs I. Critical distance between the cartilaginous eustachian tube and the internal carotid artery. Eur Arch Otorhinolaryngol 2017;274:73–7.



14. Schröder S, Lehmann M, Korbmacher D, Sauzet O, Sudhoff H, Ebmeyer J. Evaluation of tubomanometry as a routine diagnostic tool for chronic obstructive eustachian tube dysfunction. Clin Otolaryngol 2015;40:691–7.


15. Herrera M, Eisenberg G, Plaza G. Clinical assessment of eustachian tube dysfunction through the eustachian tube dysfunction questionnaire (ETDQ-7) and tubomanometry. Acta Otorrinolaringol Esp (Engl Ed) 2019;70:265–71.


16. Alper CM, Teixeira MS, Kim JH, Douglas Swarts J. Diagnostic accuracy of tubomanometry R value in detecting the eustachian tube pressure equalizing function. Eur Arch Otorhinolaryngol 2017;274:1865–72.



17. Martino E, Di Thaden R, Krombach GA, Westhofen M. Function tests for the Eustachian tube. Current knowledge. HNO 2004;52:1029–39. quiz 1040.



18. Teixeira MS, Swarts JD, Alper CM. Accuracy of the ETDQ-7 for identifying persons with eustachian tube dysfunction. Otolaryngol Head Neck Surg 2018;158:83–9.




19. McBride TP, Derkay CS, Cunningham MJ, Doyle WJ. Evaluation of noninvasive eustachian tube function tests in normal adults. Laryngoscope 1988;98(6 Pt 1):655–8.


20. Smith ME, Takwoingi Y, Deeks J, Alper C, Bance ML, Bhutta MF, et al. Eustachian tube dysfunction: a diagnostic accuracy study and proposed diagnostic pathway. PLoS One 2018;13:e0206946.



21. Smith ME, Tysome JR. Tests of eustachian tube function: a review. Clin Otolaryngol 2015;40:300–11.


22. Özgür E, Bilgen C, Cengiz Özyurt B. Turkish validity and reliability of eustachian tube dysfunction questionnaire-7. Braz J Otorhinolaryngol 2018;84:435–40.


23. Hansen LJ, Glad H, Jørkov A, Lundin K, Kirchmann M. Validating the 7-item Eustachian tube dysfunction questionnaire in Danish. Dan Med J 2020;67:A11190617

24. Menezes AS, Ribeiro DC, Guimarães JR, Costa I, Moreira F, Dias L. Translation and validation of the “7-Item Eustachian Tube Dysfunction Questionnaire” to European Portuguese (PT). Acta Med Port 2020;33:191–7.



25. Ungar OJ. The Hebrew version of the eustachian tube dysfunction questionnaire-7. Hear Balance Commun 2018;16:114–9.

26. Chen X, Xie L, Zeng H, Xu Y, Xiong H. Local versus general anesthesia for balloon dilation of the Eustachian tube: a single-center retrospective study in a Chinese population. Ear Nose Throat J 2020;May 19 [Epub]. Available at: https://doi.org/10.1177/0145561320923172.



27. Cutler JL, Meyer TA, Nguyen SA, O’Malley EM, Thackeray L, Slater PW. Long-term outcomes of balloon dilation for persistent eustachian tube dysfunction. Otol Neurotol 2019;40:1322–5.


28. Parsel SM, Unis GD, Souza SS, Bartley H, Bergeron JM, Master AN, et al. Interpretation of normal and abnormal tympanogram findings in eustachian tube dysfunction. Otolaryngol Head Neck Surg 2021;164:1272–9.



29. Lin WL, Chou YF, Sun CH, Lin CC, Hsu CJ, Wu HP. Evaluation of thirty patients with eustachian tube dysfunction in Taiwan by questionnaire survey. J Formos Med Assoc 2020;119:621–6.


30. Schröder S, Lehmann M, Sauzet O, Ebmeyer J, Sudhoff H. A novel diagnostic tool for chronic obstructive eustachian tube dysfunction—the eustachian tube score. Laryngoscope 2015;125:703–8.


31. Swarts JD, Alper CM, Luntz M, Bluestone CD, Doyle WJ, Ghadiali SN, et al. Panel 2: eustachian tube, middle ear, and mastoid--anatomy, physiology, pathophysiology, and pathogenesis. Otolaryngol Head Neck Surg 2013;148(4 Suppl):E26–36.