Introduction
It is known that the central and peripheral nervous systems are affected by coronavirus disease (COVID-19), which also causes a variety of neuro-otologic illnesses, according to scientific and clinical evidence [
1].
A minimum of three consecutive frequency losses of 30 dB within 72 hours is required for the diagnosis of sudden sensorineural hearing loss (SSNHL), which is defined as the sudden onset of sensorineural hearing loss (SNHL) without a known cause [
2]. Between 5 to 27 cases of SSNHL per 100,000 people occur annually [
3]. There is no known cause of SSNHL. However, autoimmune disease, labyrinthine membrane rupture, viral infection, circulatory abnormalities, and central nervous system defects are among the potential causes [
4,
5].
Viral infection may be the root cause of SSNHL, according to compelling evidence [
6]. It might be connected to the reactivation of latent viruses inside spiral ganglia, direct viral access to the labyrinth or the auditory nerve, or immunoregulation of systemic viral infections [
7]. Viruses like adenovirus, lasa fever, and the mumps can cause SSNHL. Increasing evidence suggests that COVID-19 patients are more likely to develop SSNHL [
8-
10]. However, there are still numerous unanswered questions regarding COVID-19-related SSNHL. The purpose of this review is to evaluate the impact of COVID-19 on the incidence of SSNHL and to provide an understanding of the clinical characteristics of COVID-19-related SSNHL.
Case Report
Case 1
A 15-year-old girl was referred 3 months after COVID-19 infection with reported hearing loss and tinnitus. She had tested normal hearing threshold before the reported hearing loss. Endoscopy of both eardrums showed no abnormal findings. The tympanogram and acoustic reflexes were normal, WeberŌĆÖs test was lateralized to the non-affected ear, and RinneŌĆÖs test at 256 Hz and 512 Hz showed air conduction greater than bone conduction on both ears. The pretreatment audiogram indicated a severe degree of SNHL to deafness (90 dB) to all frequencies of her right ear and normal findings of the left ear.
She was treated with oral methylprednisolone in a tapering form for 10 days without any improvement in the subsequent audiogram. Furthermore, she underwent 3 administrations of intratympanic dexamethasone to her affected ear. Her audiogram showed an improvement in the lower and middle frequencies (etc. 250, 500, 1,000; and 2,000 and 3,000 Hz) at about 50 dB. The girl reported complete remission of the tinnitus. She was finally referred for 15 sessions of hyperbaric oxygen therapy and when completing those, the last audiogram showed a further improvement at 250 HzŌĆō3,000 Hz to normal hearing.
A screening test for toxoplasmosis (IgG, IgM), Cytomegalovirus (CMV; IgG, IgM), Epstein-Barr virus (EBV; IgG, IgM), IgG, IgA, IgM, IgE, C4, and antinuclear antibody (ANA) was negative.
Case 2
The second case, a 14-year-old boy was presented 2 months after COVID-19 infection with reported hearing loss. He had normal tested hearing threshold before the reported hearing loss.
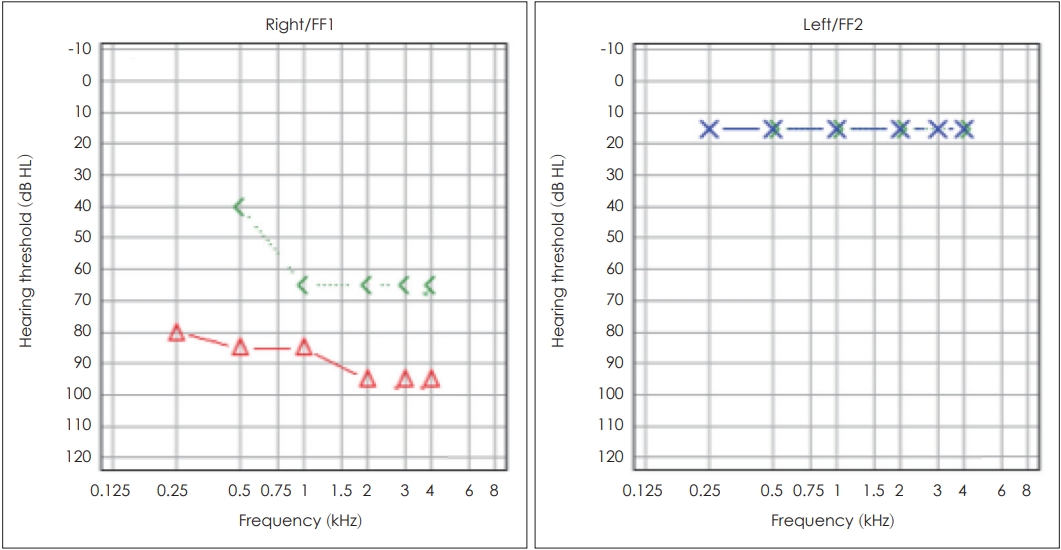
A full ENT clinical examination was performed; endoscopy of both eardrums with no abnormal findings, normal tympanogram, and acoustic reflexes, WeberŌĆÖs test was lateralized to the non-affected ear, and RinneŌĆÖs test at 256 Hz and 512 Hz showed air conduction greater than bone conduction on both ears. The pretreatment audiogram of the second case revealed a severe degree of SNHL to deafness to all frequencies of his right ear and normal findings of the left ear (
Fig. 1). He was then treated with oral methylprednisolone for 10 days and upon his reevaluation with an audiogram, an improvement was noted concerning the lower frequencies (
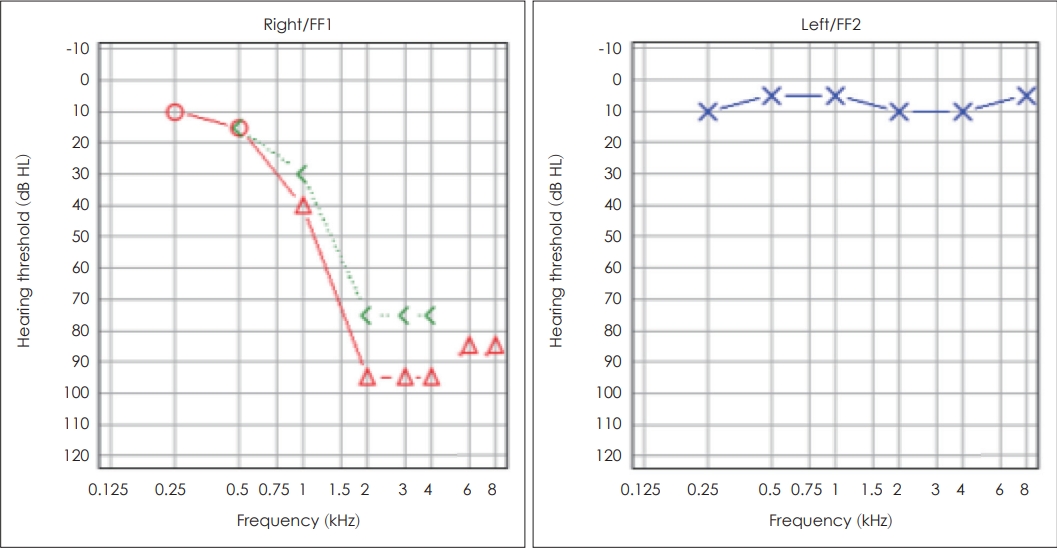
Fig. 2). He was then referred for 12 sessions of hyperbaric oxygen therapy and when completing those, the audiogram showed a further improvement of the lower and middle frequencies. He finally underwent 3 administrations of intratympanic dexamethasone to his affected ear, and his last audiogram showed a further improvement from 40 dB to 10 dB at 1,000 Hz and from 95 dB to 80 dB at 2,000 Hz (
Fig. 3). The boy reported an improvement of his day-to-day activities and way of living concerning his hearing. It is important to be noted that a screening test for toxoplasmosis (IgG, IgM), CMV (IgG, IgM), EBV (IgG, IgM), IgG, IgA, IgM, IgE, C4, and ANA was performed; ANA came back positive and he was referred to a rheumatologist for further evaluation.
Case 3
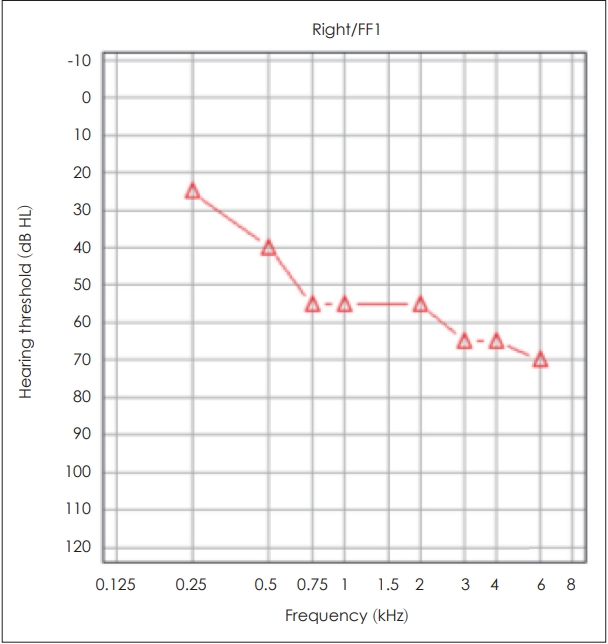
The third and most recent case, a 14-year-old boy was presented at the ENT emergency department 2 months post COVID-19 infection, with reported unilateral hearing loss. He had normal tested hearing threshold before the reported hearing loss. A full ENT clinical examination was performed. A first degree left-beating optokinetic nystagmus, compatible with right peripheral vestibulopathy was noted, WeberŌĆÖs test was lateralized to the non-affected ear, and RinneŌĆÖs test at 256 Hz and 512 Hz showed air conduction greater than bone conduction on both ears. The pretreatment audiogram of the third case showed a severe degree of SNHL to deafness to all frequencies of his right ear and normal findings of the left ear. A computed tomography (CT) with the administration of contrast agent was performed, without any abnormal findings. The boy was then admitted to the ENT clinic and received intravenous methylprednisolone in a tapering form for 10 days. Furthermore, he underwent 3 intratympanic dexamethasone injections to his affected ear (starting on the 3rd day of hospitalization and with a 2-day gap in-between). He then continued receiving oral methylprednisolone for 7 more days, underwent 12 sessions of hyperbaric oxygen therapy and a magnetic resonance imaging (MRI) scan with the administration of a contrast agent, without any abnormal findings. Upon the course of his treatment, the audiogram reevaluation showed a similar course as the second case; a significant improvement in the lower frequencies and a mild improvement in the middle frequencies (
Fig. 4). The boyŌĆÖs history revealed a congenital hypothyroidism from birth and was treated with thyroxin administration for the first 18 months of his life, with normal hormonal check-ups ever since. Screening tests during his hospitalization showed a slight elevation of thyroid stimulating hormone (TSH) and was referred to an endocrinologist for further evaluation.
Table 1 compares these three cases.
Since all cases were children with body mass of over 50 kg, they were administered doses given to adults, concerning oral, intravenous, and intratympanic glucocorticoids. To be more precise, for oral administration, 16 mg of methylprednisolone tablets were given in a tapering form; S: 3├Ś1 for 3 days, S: 2├Ś1 for the next 3 days, and S: 1├Ś1 for the last 3 days. Furthermore, the intravenous dose was 1 mg/kg/day prednisolone for 7 days followed by 0.5 mg/kg/day for 3 days; (after his discharge the third case continued taking orally methylprednisolone 32 mg/day for 4 days, followed by 16 mg/day for an additional 3 days). As for the intratympanic injections, 0.6 mL of 4 mg/mL dexamethasone was administered. The coadministration of a proton pump inhibitor is of great importance.
Discussion
The audio-vestibular system may be infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), leading to SSNHL [
1]. However, the precise processes by which SARS-CoV-2 affects the audio-vestibular system are still not well understood. Despite the fact that several investigations into COVID-19-related SSNHL have been carried out, they have been dispersed and unorganized. The true frequency of SSNHL in COVID-19 patients is worldwide unknown [
7]. The preferred treatment for COVID-19-related SSNHL is glucocorticoids [
4]. When hearing loss is suspected in patients with a positive history of COVID-19 illness, hearing testing is advised. If SSNHL is found, quick and aggressive treatment is crucial. In the available literature, pure tone audiometry is mainly used to detect COVID-19-related SSNHL. Speech audiometry may be considered to evaluate the effect of SARS-CoV-2 on cognitive processes [
6].
It is crucial to look into this further given the prevalence of the coronavirus in the general population and the severe morbidity of adult hearing loss. This is particularly true considering the urgent need to detect and treat hearing loss and the existing accessibility issues to healthcare. We advise urgent referral to otolaryngology for any patient presenting with acute hearing loss.
ENT clinical examination of all our cases was normal. Endoscopy of the eardrums showed no pathological signs. The tympanogram and the acoustic reflexes were normal in both ears in all cases. WeberŌĆÖs was lateralized to the non-affected ear and RinneŌĆÖs test at 256 Hz and 512 Hz showed air conduction greater than bone conduction on both ears. Only the third child had an additional first degree left-beating optokinetic nystagmus, compatible with right peripheral vestibulopathy. The audiogram indicated unilateral severe SSNHL in all frequencies. CT and MRI scans of the brain and temporal bones showed no pathology of the related structures. Oral methylprednisolone was administered to the first 2 cases and intravenous methylprednisolone in a tapering form was administered to the third patient, respectively. In addition, the children underwent intratympanic dexamethasone injections and hyperbaric oxygen therapy with hearing improvement in lower and middle frequencies.
The increase in cases of SSNHL post-COVID-19 infection referred to our hospital, ever since the outbreak of the SARS-CoV-2 pandemic, combined with the fact that the incidence of sudden hearing loss in the pre-pandemic years was relatively low, may suggest the COVID-19 infection as a possible cause.
The limitation of our paper is the small number of cases due to the recent COVID-19 pandemic infection. Worldwide multicenter studies in children should be conducted to investigate the exact impact of COVID-19-related SSNHL in pediatric population.
We report the first cases of SSNHL in COVID-19 pediatric patients around the world to date. The prognosis of COVID-19-related SSNHL in children is closely related to the onset of treatment. The combination of glucocorticoids, intratympanic dexamethasone, and hyperbaric oxygen therapy could be effective for COVID-19-related SSNHL in children. Further large-scale, multicenter studies in children should be conducted to investigate the pathophysiology, diagnosis, treatment, and prognosis of COVID-19-related SSNHL in pediatric population.