 |
 |
- Search
| J Audiol Otol > Volume 28(2); 2024 > Article |
|
Abstract
We herein review the use of electrocochleography (ECoG) to assess peripheral auditory system responsiveness in a growing population of cochlear implant (CI) users with preserved hearing in ears with implants. Twenty-eight recently published intracochlear ECoG articles were thoroughly reviewed to investigate the prognostic utility of intraoperative ECoG monitoring to assess hearing preservation, and the clinical applicability of postoperative ECoG for estimating audiometric thresholds and monitoring longitudinal changes in residual acoustic hearing in patients with EAS. Intraoperative ECoG studies have focused on monitoring the changes in the cochlear microphonics (CM) amplitudes during and after electrode insertion. Mixed results have been reported regarding the relationship between changes in CM amplitude in the operating room and changes in hearing thresholds after surgery. Postoperative ECoG studies have shown that CM and auditory nerve neurophonics thresholds correlate significantly with behavioral thresholds. ECoG thresholds sensitively detect changes as residual acoustic hearing decreases over time in some CI users. This indicates its potential clinical value for monitoring the post-implantation status of the peripheral auditory system. Intracochlear ECoG can provide real-time intraoperative feedback and monitor postoperative hearing preservation in a growing population of CI users.
During the past few decades, cochlear implants (CIs) have become a successful (re)habilitation option to restore hearing sensitivity in people with severe to profound sensorineural hearing loss. Recently, the CI candidacy criteria have been significantly relaxed to include individuals with good lowfrequency hearing but substantial bilateral, high-frequency hearing loss [1-4]. These individuals with severe to profound high-frequency hearing loss often do not receive sufficient benefits from conventional amplification [5]. For this population, combined electro-acoustic stimulation (EAS) appears to be a viable option compared to conventional cochlear implantation, which can result in complete loss of residual hearing. The less traumatic CI electrode array design and the use of the “soft surgery” technique allow for the preservation of residual low-frequency acoustic hearing. EAS, also called “hybrid CI,” is designed to provide both electric and acoustic stimulation to the same ear. The electrode array provides high-frequency electric stimulation, while an integrated hearing aid provides amplification for low-frequency sounds. Preserving acoustic hearing has benefits, including improved speech performance in background noise and music perception when listeners use combined acoustic and electric stimulation compared with those using electric stimulation alone [1-3,6].
Individuals eligible for EAS are more likely than those without residual hearing to have preserved structures, including surviving hair cells and auditory nerve fibers near the apex of the cochlea after cochlear implantation. Interest in the role played by the peripheral auditory system in driving outcomes with a CI has grown along with this population of users. For CI users with residual acoustic hearing, responses from the cochlea to acoustic stimuli can be recorded using the electrocochleography (ECoG) technique. ECoG has proved to be a valuable tool for measuring the function of the auditory periphery and has been clinically applied in diagnosing and monitoring hearing and balance disorders [7,8]. Recently, there has been growing interest in recording ECoG responses from CI users with preserved hearing for intraoperative and postoperative monitoring purposes [9-12]. This review summarizes studies about the use of ECoG to assess the response of the peripheral auditory system in CI users who have residual acoustic hearing in the implanted ear.
ECoG is a technique that has been used for decades to record responses from cochlear hair cells and the auditory nerve [7]. A recording obtained using ECoG, an electrogram, is a composite response that includes contributions from hair cells (i.e., the cochlear microphonic [CM] and summating potential [SP]) and the auditory nerve (i.e., the compound action potential [CAP] and auditory nerve neurophonic [ANN]). This complex of responses, collectively called ECoG, provides a rich source of information about the survival of functional cochlear elements and may help understand underlying pathophysiology related to the peripheral auditory system. An example ECoG waveform recorded using a low-frequency tone burst is shown in Fig. 1.
ECoG has been used in clinical settings to support the diagnosis and assessment of Meniere’s disease, to enhance wave I of the auditory brainstem response, to assist with the diagnosis of auditory neuropathy spectrum disorders, and to monitor cochlear and auditory nerve function during surgery [13-15]. During the past 30 years, ECoG has been an excellent tool for diagnosing patients with Meniere’s disease/endolymphatic hydrops [7,8]. ECoG recordings from patients with Meniere’s disease are characterized by an enlarged SP and SP/action potential ratio, compared with normal hearing ears, due to an increase in the endolymphatic volume that creates mechanical biasing of vibration in the organ of Corti and amplifies the SP [13,14]. An interest in ECoG as a diagnostic tool has surged again since 2010 due to its potential ability to mitigate possible intracochlear damage and monitor hearing preservation in CI users post-implant.
Since hearing preservation became possible for CI users through the development of thinner, more flexible electrode arrays and the use of soft surgical techniques, several research groups have become interested in the possibility of using ECoG to measure cochlear function in this growing population of CI recipients. Among the various components of the composite ECoG response, the focus was on identifying the CM and ANN (Fig. 1). CAPs and SPs are often challenging to identify in these recordings [9,16]. The common technique used to segregate hair cells and neural components involves recording the response using condensation and rarefaction stimulus polarities. The CM reverses polarity when the stimulus polarity is reversed. Neural components, generally assumed to reflect postsynaptic responses, do not. By adding responses recorded using condensation and rarefaction tone bursts (the “summed” response), the hair cell response (e.g., the CM) can be minimized, and the neural response (CAP and ANN) enhanced. By subtracting the responses recorded using opposite stimulus polarities (the “difference” response), the CM is enhanced, and neural responses (CAP and ANN) are minimized. Fig. 2 shows an example of CM and ANN responses from a single CI user with residual acoustic hearing [17]. The stimulus was a 750 Hz tone burst presented at 116 dB ppeSPL. The top panel shows the “difference” response, and the bottom panel shows the “summed” response. The CM is enhanced in the top panel, showing oscillations at approximately 750 Hz. The neural responses (CAP and ANN) are evident in the bottom panel. The ANN is a sinusoidal potential that oscillates at twice the stimulus frequency (i.e., 1,500 Hz).
The ECoG technique is increasingly being used to monitor the status of residual hearing during CI surgery [12,18-22]. In most intraoperative ECoG studies, the primary focus was monitoring the CM, which was preferred due to its robust and large response magnitude, compared with the ANN. Also, it can be recorded in most EAS users, which makes interpretation much easier. Moreover, the CM is generated by hair cells, which are likely to be the site of damage in the cochlea if insertion trauma occurs during cochlear implantation.
ECoG responses can be recorded noninvasively from an electrode inside the cochlea, known as intracochlear ECoG. Proximity to the generating source could be a significant advantage of this technique, which uses the reverse telemetry capabilities of the CI [9-11]. The reverse telemetry system was designed to sample the voltage across a pair of electrodes after a stimulus to measure peripheral neural function, and it is commonly used to record the electrically evoked CAP. The action potentials that result from a stimulus are recorded from the intracochlear electrode, amplified, sampled, and encoded for transmission via the radio frequency link back to the speech processor. The voltage waveforms recorded are then averaged and processed offline using the software that controls the telemetry system. This bidirectional telemetry system is available for all three major CI devices using different names: the neural response telemetry (NRT, Cochlear Ltd.), neural response imaging (NRI, Advanced Bionics), and auditory nerve response telemetry (ART, MED-EL).
Intracochlear ECoG via the reverse telemetry system has been used to offer real-time feedback about cochlear responses during electrode insertion [10,11,23-28]. The prognostic value of intracochlear ECoG recordings during CI surgery was investigated to determine whether these recordings can be used to assess insertion trauma and predict early postoperative hearing preservation. Mixed results were reported on the relationship between changes in the ECoG response and hearing preservation. One early study showed that the newly developed intracochlear ECoG method using the NRT system of the Nucleus CI (Cochlear Ltd., NSW, Australia) feasibly provided real-time feedback for monitoring changes in CM amplitudes as the site of recording progressed from the base of the cochlea toward the location where the cochlea is the most sensitive to the stimulus [10,11]. Subjects who showed stable CM amplitudes at the end of the recording procedure were more likely than others to have preserved hearing afterward. Subjects with preserved CM at the end of insertion had, on average, 15 dB better low-frequency acoustic hearing than subjects with a transient or permanent reduction in CM amplitudes during the insertion process. Conversely, a few studies have shown a less clear relationship between the ECoG response and hearing preservation [18,28]. CM amplitude dropped on average 3 dB (range 0–8 dB) during electrode insertion in 13 subjects, who all received the Advanced Bionics Mid-Scala electrode array (Advanced Bionics, Valencia, CA, USA) [28]. However, neither a CM amplitude drop from the round window to peak amplitude nor a drop from the peak to the end of insertion correlated significantly with a postoperative behavioral audiometric threshold shift at low frequencies (125–500 Hz).
Recently, several studies with relatively large sample sizes investigated the usefulness of intracochlear ECoG as a realtime monitoring tool for hearing preservation [24,25,27]. One multicenter study recruited 68 EAS users with the Advanced Bionics HiFocus MidScala or SlimJ electrode arrays from five high-volume CI centers and reported wide individual variability in ECoG drop patterns during electrode insertion and a moderate positive correlation (r=0.56, p<0.0001) between the magnitude of the ECoG drop and pure-tone average (PTA) changes in the pre- to postoperative audiometric thresholds [27]. Another multicenter study recruited 47 EAS users with the Advanced Bionics hearing preservation arrays from 10 tertiary CI centers and reported an average of 27 dB of low-frequency PTA (LF-PTA) changes in intraoperative ECoG monitoring during CI electrode insertion [25]. Among those subjects, 34.5% showed “good” hearing preservation (LF-PTA change 0–15 dB), 22.5% showed “fair” preservation (LF-PTA change >15–29 dB), and 43.5% showed “poor” preservation (LF-PTA change ≥30 dB) at low frequencies, indicating wide individual variability in post-op residual hearing. Furthermore, that study population did not find significantly better hearing preservation in patients with audible ECoG monitoring available to the surgeon during electrode insertion than in those whose surgeries were conducted without audible ECoG monitoring. Another study recruited 47 EAS patients with the Advanced Bionics Slim J or MidScala electrode arrays and recorded intracochlear ECoG while allowing the surgeon to adjust the course of the electrode insertion based on CM drops [24]. No significant correlation was observed between a CM amplitude drop and LF-PTA changes between the pre- and postoperative audiometric thresholds. Three ECoG response amplitude patterns were observed: growth, fluctuation, and total loss. Subjects with the growth amplitude pattern showed the smallest postoperative hearing loss, and subjects with fluctuating amplitudes showed no meaningful correlation between the ECoG responses and postoperative hearing change. When considering the phase of the CM in addition to the amplitude, the groups with no CM drop in amplitude or a CM drop with a concurrent phase shift showed better hearing preservation, whereas subjects who showed a CM drop without a concurrent phase shift had more surgery-induced hearing loss. These mixed results from several studies indicate that CM amplitude alone might not be insufficient to detect damage or insertion trauma. Taking both the phase and amplitude into account might identify ECoG amplitude drops caused by touching or damaging the basilar membrane batter than simple ECoG amplitude drops because the recording electrode has just passed the generator. However, more data are needed to optimize the usefulness of ECoG in preventing intraoperative cochlear damage during electrode insertion [24].
Intraoperative ECoG recordings have also been used to provide information about the scalar location of the electrode array during and after electrode insertion. Previous studies reported frequent instances of translocation from the scala tympani (ST) to the scala vestibuli (SV) during electrode insertion (e.g., 22% in Koka, et al. [29], 38% in O’Connell, et al. [28]) and the negative effects of such location changes on speech outcomes [30]. Recent data compared the final electrode scalar location, and it differed between subjects with and without audible ECoG monitoring [25]. Seven percent of subjects (3 of 21) without audible ECoG monitoring showed electrode translocation from the ST into the SV. In contrast, all 22 patients with audible ECoG monitoring had electrodes that stayed completely within the ST, with no translocations observed, indicating the ability of intracochlear ECoG monitoring to identify the final electrode scalar location. A retrospective review of intraoperative ECoG showed that all subjects whose electrode arrays translocated from the ST to the SV showed a sizeable decrease in CM amplitudes during insertion without recovery, though this CM amplitude change did not differ significantly from the responses of the non-translocation group [28,29,31]. On the other hand, the differences between the intraoperative CM thresholds and postoperative audiometric thresholds for patients with electrodes that crossed from the ST to the SV were significantly lower than those for patients whose electrodes stayed in the ST, which suggests that scalar translocation from the ST to the SV is associated with significantly higher shifts in low-frequency audiometric thresholds than are found when the electrodes are inserted entirely within ST [28]. In addition, incorporating phase changes during electrode insertion appeared to correctly estimate the electrode position in 82% of cases and enhanced the specificity and sensitivity of predicting scalar translocation using intraoperative ECoG monitoring [29]. Preliminary data reveal a trend of smaller phase changes in the translocation group and larger phase shifts in the non-translocation group, although the underlying physiologic mechanism behind the phase shift is not yet clear. Taken together, the still preliminary data suggest that intracochlear ECoG might be good for detecting scalar translocation and could help surgeons achieve a lower rate of scalar translocation. Further studies with larger samples are needed to test the validity of using combined CM amplitude and phase information to predict electrode scalar location.
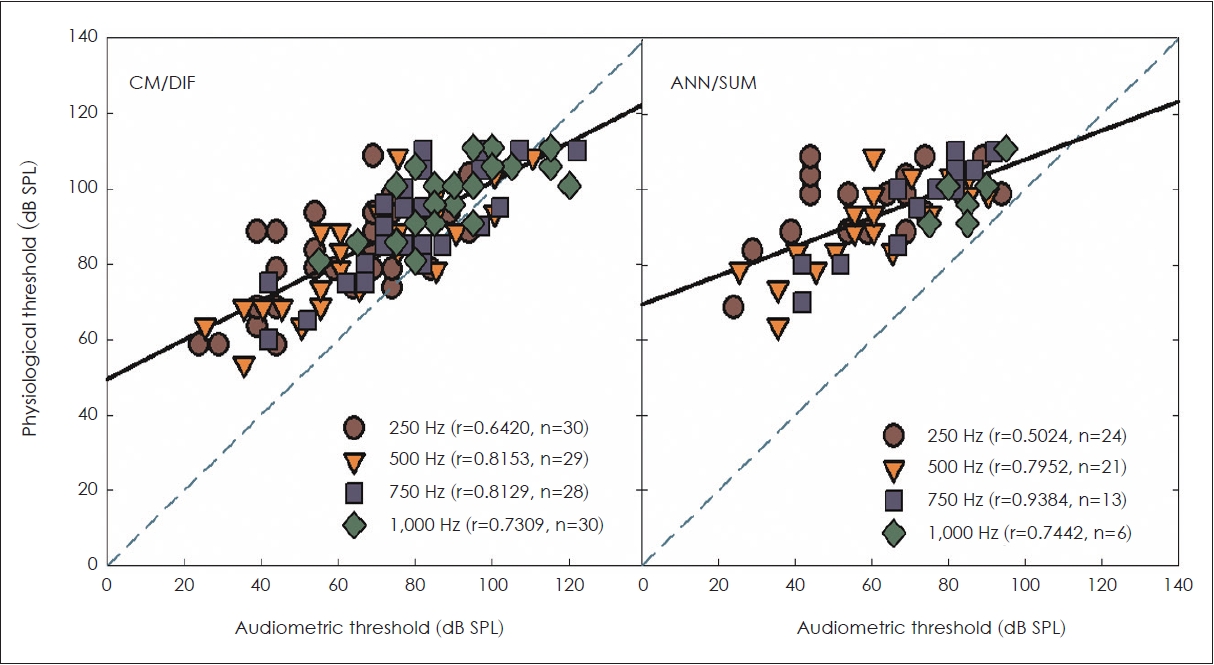
ECoG responses can be recorded from an intracochlear electrode at any time after surgery in CI users with preserved acoustic hearing [9,10,17,28,29]. The most widely studied clinical application of postoperative ECoG is for estimating behavioral thresholds based on electrophysiologic thresholds. Abbas, et al. [9] demonstrated the feasibility of a noninvasive method that used standard clinical software (Nucleus Custom Sound EP) and the NRT system to record ECoG responses from Nucleus Hybrid CI users. Both the CM and ANN responses were identified from most EAS subjects. CM and ANN thresholds measured with a 500 Hz tone burst correlated significantly with postoperative behavioral thresholds at 500 Hz [9]. When extended to other frequencies, the CM and ANN thresholds correlated significantly with audiometric thresholds at 250, 750, and 1,000 Hz (Fig. 3) [17,32]. Strong correlations between the CM and ANN thresholds and the postoperative behavioral thresholds were replicated in other studies using the ECoG research module developed by Advanced Bionics [26,28]. Good correlations between electrophysiological thresholds and behavioral thresholds suggest the validity of intracochlear ECoG as a tool to estimate audiometric thresholds, which could be helpful in hard-to-test populations such as very young children and individuals with additional disabilities.
Another clinical application of postoperative ECoG is monitoring for changes in preserved acoustic hearing over time. Despite efforts to preserve cochlear structures and acoustic hearing by using soft surgical techniques and carefully designed electrodes, patients who were implanted with hearing preservation electrode arrays often experienced 10–15 dB of acoustic hearing decrease in the implanted ear immediately after surgery [1,33]. In the small population of CI users with residual acoustic hearing, delayed onset hearing loss generally occurs within the first year of CI use [34,35]. Among the CI users with a Nucleus Hybrid S8 electrode, 20% experienced an average of 24 dB of hearing loss several months after surgery in addition to hearing loss documented at the initial activation of the CI [34]. A retrospective chart review of CI patients with hearing preservation arrays also revealed that 38% (32 out of 85) of adult Nucleus Hybrid CI users presented delayed hearing loss of various degrees and rates, and the progression of hearing loss was rapid in most of those cases (26 out of 32) [35]. For individuals with delayed onset hearing loss, significantly elevated CM and ANN thresholds have been reported as their acoustic hearing changed over time [9,17]. In addition to subjects with a significant hearing drop, several subjects who experienced less significant hearing loss (less than 10 dB change in PTA at 250–1,000 Hz) also showed notable increases in the CM and ANN thresholds [9,17]. Therefore, ECoG recordings are sensitive enough to reflect the pattern of changes in residual acoustic hearing, which indicates their potential clinical value in monitoring changes in the status of the peripheral auditory system post-implant. Interestingly, in some EAS users who lost their residual acoustic hearing completely, the CM response was still measurable, though the magnitude of CM responses was significantly reduced compared with pre-hearing loss, but the ANN response was totally absent after delayed hearing loss [36]. Smaller but measurable CM with absent ANN in patients with a total loss of residual hearing implies the existence of some viable hair cell function in this population, but synaptic disconnection between the hair cells and nerve fibers might compromise the encoding of auditory stimulation to the auditory nerve. Having differential metrics to reflect the status of hair cells (CM) and the auditory nerve (ANN) could help to elucidate the pathophysiology of delayed hearing loss and be used to characterize the status of the auditory periphery. A preliminary study of genetic hearing loss investigated an electrophysiological application to assess the functional effects of a genetic lesion on the peripheral auditory system [37]. When intracochlear ECoG was performed in eight EAS users to assess their hair cell and neural function, three subjects with pathogenic variants in TMPRSS3 that would affect spiral ganglion neurons and five subjects with pathogenic variants in genes affecting the cochlear sensory partition did not differ in their CM responses. However, the ANN responses were significantly smaller in subjects with TMPRSS3 deafness than in subjects in the sensory group. These results suggest a new role for intracochlear ECoG: specifying the site of a lesion in the peripheral auditory system that is not available from behavioral testing and elucidating the underlying pathophysiology associated with the causes or etiologies of delayed onset hearing loss that some CI users with residual acoustic hearing often experience [37,38].
Most intracochlear ECoG studies reviewed here used custom ECoG software specifically designed for research or clinically available software with a research patch to enable the collection of intracochlear recordings from CI users [2,9-11,17-19,23,24,26,28,29,32,36,37]. All major CI manufacturers (Cochlear Ltd., Advanced Bionics, MED-EL) have developed research ECoG software; however, the use of those systems for clinical trials was restricted to a few CI research centers in the United States and Europe. Using the research software certainly requires time and effort because the audiologist has to be trained to conduct and interpret ECoG results reliably. That restriction could limit the potential use of ECoG as a routine clinical procedure to monitor the hearing status of CI users with EAS. Recently, there has been an effort to commercialize the ECoG system for easy clinical use. Advanced Bionics launched the AIMTM (Active Insertion Monitoring) system, which was approved by the US Food and Drug Administration (FDA) in 2019. This system allows real-time ECoG monitoring during CI surgery and can estimate postoperative audiometric thresholds across frequencies based on an ECoG analysis algorithm. Compared with the research software, this clinical version of the ECoG system is simplified, automated, and portable, which allows faster and more efficient implementation without patient collaboration. Objective measurements of audiometric thresholds based on ECoG measurements might also help audiologists working with very young or other hard-to-test populations. Recently, several multicenter studies with significantly large sample sizes reported results of intracochlear ECoG recorded via the commercially available AIM system, and supported the prognostic value of using intracochlear ECoG to guide surgical decision-making during CI surgery and thereby promote hearing preservation in CI users with residual acoustic hearing [24,25,27].
ECoG is a widely used clinical tool that provides rich information about the auditory periphery, including cochlear hair cells and the auditory nerve. It might be helpful in many circumstances, particularly using two components (e.g., CM and ANN) to identify the site of a lesion, assist in differential diagnosis (i.e., presynaptic vs. postsynaptic), and understand the considerable variance in the postoperative performance of CI users. Along with growing efforts to provide innovative electrode designs that can preserve cochlear structures and reduce the trauma of CI surgery, ECoG appears to be useful tool that can promote hearing preservation for CI patients. ECoG has proved to be feasible for providing real-time feedback intraoperatively and monitoring the status of hearing preservation postoperatively. This review shows how this long-standing diagnostic tool has been successfully applied to the new CI population. Further studies are required to make this technique more clinically accessible and understand how ECoG correlates with the prognosis for postoperative CI outcomes.
Acknowledgments
This study was presented as a featured talk at the 14th Asia Pacific Symposium on Cochlear Implant and Related Sciences (APSCI 2023) (November 8-11, 2023, Seoul, Korea).
Fig. 1.
An example of electrocochleography responses (electrogram) recorded using a 500 Hz tone burst. CM, cochlear microphonic; ANN, auditory nerve neurophonic; CAP, compound action potential; SP, summating potential.

Fig. 2.
An example of CM and ANN recordings from a single CI user. CM, cochlear microphonic; CI, cochlear implant; DIF, difference response; ANN, auditory nerve neurophonic; SUM, summed response; CAP, compound action potential. Data excerpted from Kim et al. Hear Res 2018;370:304-15 [17].
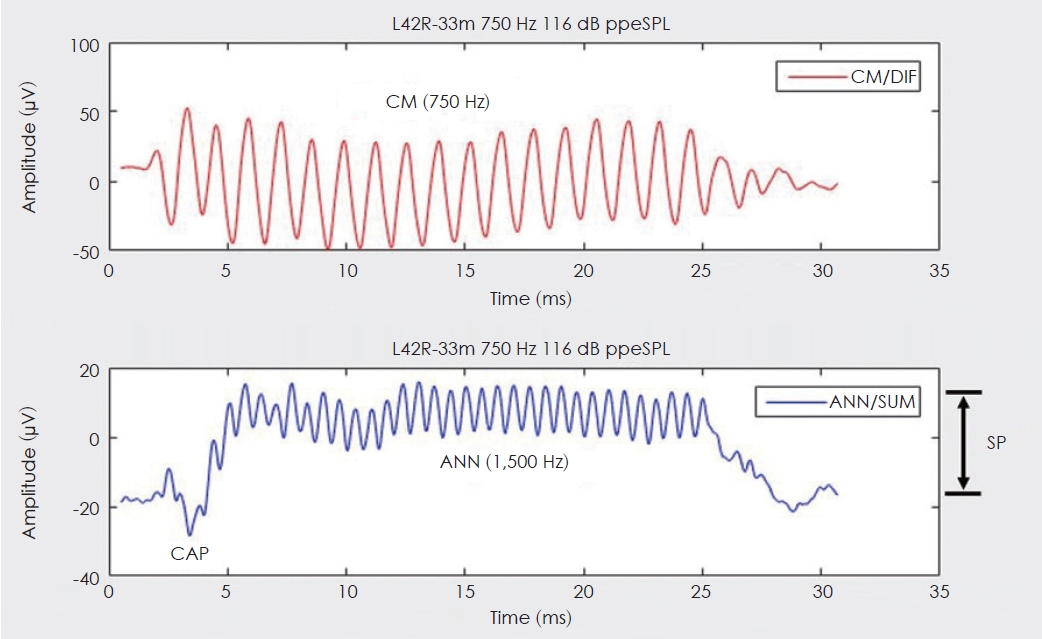
Fig. 3.
Correlations between electrocochleography thresholds and postoperative audiometric thresholds. CM, cochlear microphonic; DIF, difference response; ANN, auditory nerve neurophonic; SUM, summed response. Data excerpted from Kim et al. Hear Res 2018;370:304- 15 [17].
REFERENCES
1. Gantz BJ, Hansen MR, Turner CW, Oleson JJ, Reiss LA, Parkinson AJ. Hybrid 10 clinical trial: preliminary results. Audiol Neurootol 2009;14(Suppl 1):32–8.

2. Pillsbury HC 3rd, Dillon MT, Buchman CA, Staecker H, Prentiss SM, Ruckenstein MJ, et al. Multicenter US clinical trial with an electricacoustic stimulation (EAS) system in adults: final outcomes. Otol Neurotol 2018;39:299–305.



3. Roland JT Jr, Gantz BJ, Waltzman SB, Parkinson AJ. United States multicenter clinical trial of the cochlear nucleus hybrid implant system. Laryngoscope 2016;126:175–81.




4. Roche JP, Hansen MR. On the horizon: cochlear implant technology. Otolaryngol Clin North Am 2015;48:1097–116.


6. Gfeller KE, Olszewski C, Turner C, Gantz B, Oleson J. Music perception with cochlear implants and residual hearing. Audiol Neurootol 2006;11(Suppl 1):12–5.



8. Ferraro JA. Electrocochleography: a review of recording approaches, clinical applications, and new findings in adults and children. J Am Acad Audiol 2010;21:145–52.


9. Abbas PJ, Tejani VD, Scheperle RA, Brown CJ. Using neural response telemetry to monitor physiological responses to acoustic stimulation in hybrid cochlear implant users. Ear Hear 2017;38:409–25.



10. Campbell L, Kaicer A, Briggs R, O’Leary S. Cochlear response telemetry: intracochlear electrocochleography via cochlear implant neural response telemetry pilot study results. Otol Neurotol 2015;36:399–405.

11. Campbell L, Kaicer A, Sly D, Iseli C, Wei B, Briggs R, et al. Intraoperative real-time cochlear response telemetry predicts hearing preservation in cochlear implantation. Otol Neurotol 2016;37:332–8.


12. Fitzpatrick DC, Campbell AP, Choudhury B, Dillon MT, Forgues M, Buchman CA, et al. Round window electrocochleography just before cochlear implantation: relationship to word recognition outcomes in adults. Otol Neurotol 2014;35:64–71.


13. Gibson WP, Moffat DA, Ramsden RT. Clinical electrocochleography in the diagnosis and management of Meneère’s disorder. Audiology 1977;16:389–401.

14. Schmidt PH, Eggermont JJ, Odenthal DW. Study of Menière’s disease by electrocochleography. Acta Otolaryngol Suppl 1974;316:75–84.


15. Starr A, Sininger Y, Nguyen T, Michalewski HJ, Oba S, Abdala C. Cochlear receptor (microphonic and summating potentials, otoacoustic emissions) and auditory pathway (auditory brain stem potentials) activity in auditory neuropathy. Ear Hear 2001;22:91–9.


16. Scott WC, Giardina CK, Pappa AK, Fontenot TE, Anderson ML, Dillon MT, et al. The compound action potential in subjects receiving a cochlear implant. Otol Neurotol 2016;37:1654–61.



17. Kim JS, Tejani VD, Abbas PJ, Brown CJ. Postoperative electrocochleography from hybrid cochlear implant users: an alternative analysis procedure. Hear Res 2018;370:304–15.



18. Adunka OF, Giardina CK, Formeister EJ, Choudhury B, Buchman CA, Fitzpatrick DC. Round window electrocochleography before and after cochlear implant electrode insertion. Laryngoscope 2016;126:1193–200.




19. Choudhury B, Fitzpatrick DC, Buchman CA, Wei BP, Dillon MT, He S, et al. Intraoperative round window recordings to acoustic stimuli from cochlear implant patients. Otol Neurotol 2012;33:1507–15.



20. Dalbert A, Huber A, Veraguth D, Roosli C, Pfiffner F. Assessment of cochlear trauma during cochlear implantation using electrocochleography and cone beam computed tomography. Otol Neurotol 2016;37:446–53.


21. Dalbert A, Pfiffner F, Hoesli M, Koka K, Veraguth D, Roosli C, et al. Assessment of cochlear function during cochlear implantation by extra- and intracochlear electrocochleography. Front Neurosci 2018;12:18



22. Formeister EJ, McClellan JH, Merwin WH 3rd, Iseli CE, Calloway NH, Teagle HF, et al. Intraoperative round window electrocochleography and speech perception outcomes in pediatric cochlear implant recipients. Ear Hear 2015;36:249–60.


23. Bester CW, Campbell L, Dragovic A, Collins A, O’Leary SJ. Characterizing electrocochleography in cochlear implant recipients with residual low-frequency hearing. Front Neurosci 2017;11:141



24. Buechner A, Bardt M, Haumann S, Geissler G, Salcher R, Lenarz T. Clinical experiences with intraoperative electrocochleography in cochlear implant recipients and its potential to reduce insertion trauma and improve postoperative hearing preservation. PLoS One 2022;17:e0266077.



25. Harris MS, Koka K, Riggs WJ, Saleh S, Holder JT, Dwyer RT, et al. Can electrocochleography help preserve hearing after cochlear implantation with full electrode insertion? Otol Neurotol 2022;43:789–96.


26. Koka K, Saoji AA, Litvak LM. Electrocochleography in cochlear implant recipients with residual hearing: comparison with audiometric thresholds. Ear Hear 2017;38:e161–7.


27. Lenarz T, Buechner A, Gantz B, Hansen M, Tejani VD, Labadie R, et al. Relationship between intraoperative electrocochleography and hearing preservation. Otol Neurotol 2022;43:e72–8.



28. O’Connell BP, Holder JT, Dwyer RT, Gifford RH, Noble JH, Bennett ML, et al. Intra- and postoperative electrocochleography may be predictive of final electrode position and postoperative hearing preservation. Front Neurosci 2017;11:291


29. Koka K, Riggs WJ, Dwyer R, Holder JT, Noble JH, Dawant BM, et al. Intra-cochlear electrocochleography during cochear implant electrode insertion is predictive of final scalar location. Otol Neurotol 2018;39:e654–9.



30. Wanna GB, Noble JH, Gifford RH, Dietrich MS, Sweeney AD, Zhang D, et al. Impact of intrascalar electrode location, electrode type, and angular insertion depth on residual hearing in cochlear implant patients: preliminary results. Otol Neurotol 2015;36:1343–8.


31. Riggs WJ, Dwyer RT, Holder JT, Mattingly JK, Ortmann A, Noble JH, et al. Intracochlear electrocochleography: influence of scalar position of the cochlear implant electrode on postinsertion results. Otol Neurotol 2019;40:e503–10.



32. Tejani VD, Kim JS, Etler CP, Skidmore J, Yuan Y, He S, et al. Longitudinal electrocochleography as an objective measure of serial behavioral audiometry in electro-acoustic stimulation patients. Ear Hear 2023;44:1014–28.



33. Gantz BJ, Dunn C, Oleson J, Hansen M, Parkinson A, Turner C. Multicenter clinical trial of the Nucleus Hybrid S8 cochlear implant: final outcomes. Laryngoscope 2016;126:962–73.




34. Kopelovich JC, Reiss LA, Oleson JJ, Lundt ES, Gantz BJ, Hansen MR. Risk factors for loss of ipsilateral residual hearing after hybrid cochlear implantation. Otol Neurotol 2014;35:1403–8.



35. Scheperle RA, Tejani VD, Omtvedt JK, Brown CJ, Abbas PJ, Hansen MR, et al. Delayed changes in auditory status in cochlear implant users with preserved acoustic hearing. Hear Res 2017;350:45–57.



36. Tejani VD, Kim JS, Oleson JJ, Abbas PJ, Brown CJ, Hansen MR, et al. Residual hair cell responses in electric-acoustic stimulation cochlear implant users with complete loss of acoustic hearing after implantation. J Assoc Res Otolaryngol 2021;22:161–76.











